Drug-Induced Steven Johnson Syndrome in A 4-Year Old Boy: A Case Report- Juniper Publishers
Juniper Publishers-Open Access Journal of Dentistry & Oral Health
Abstract
Steven Johnson syndrome (SJS) is a severe variant of Erythema Multiforme (EM), typically it manifests on the skin and mucous membranes with clinical sign and symptoms of rashes, blisters or erosions on the skin covering less than 10% of the body’s surface area, and one of the most debilitating adverse drug reactions (ADR’s) recognized with high mortality rate. So early diagnosis of SJS is essential for proper management to prevent complications and reduce mortality. The aim of the present article is to enlighten the clinical features and management of SJS due to ADR in a 4-year old boy.
Keywords: Adverse drug reactions, Erythema multiforme, Blisters, Drug eruptions
Introduction
With emergence of different pathologies in modern era, there is an increasing demand for new drugs for therapeutics, resulting in drug resistance, drug intolerance and adverse drug reactions. An adverse drug reaction (ADR) may be defined as an undesirable clinical manifestation resulting from administration of a particular drug; this includes reactions due to overdose, predictable side effects and unanticipated adverse manifestations [1]. ADRs are one of the common causes of death in 0.3% to 7% of hospitalized patients [2]. Drug eruptions vary from mild rashes to severe form like Steven Johnson syndrome (SJS) and Toxic epidermal necrolysis (TEN). The drugs like antimicrobials, analgesics and antiepileptics cause SJS, which is a severe life threatening mucocutaneous syndrome [3]. Most of the SJS cases were reported in the age group of 20-50 years and less than 25% cases below 20 years and above 50 years [2]. Here with we report a case of drug-induced SJS with clinical presentations and management in a 4 year old boy.
Case Report
A 4 years old boy reported to the department with a chief complaint of bleeding from the lips since 10 days. Patient’s attendant revealed that he was asymptomatic 15 days back, later developed fever for which he was prescribed penicillin injections by a local registered medical practitioner (RMP) following which he developed blisters on his lips leading to erosion. This later started to bleed and was associated with pain, difficulty inspeech and mastication. Patient’s attendant also gave history of lesions on his extremities, genitals and irritation with discharge from eyes. General physical examination revealed multiple well-circumscribed flat lesions involving extremities, trunk, back and genitals measuring about 0.5cm to 2cms in size (Figure 1). All the vital signs were within normal range. Extraoral examination revealed erythematous eyes with discharge, bleeding from lips with extensive erosions, and restricted mouth opening (10mm) (Figure 2). On intra oral examination similar erosions were found on right and left buccal mucosa, labial mucosa and gingiva. Based on the history and clinical examination a diagnosis of Steven Johnson Syndrome was considered with a differential diagnosis of erythema multiforme major (drug induced), pemphigus vulgaris and bullous pemphigoid.


Routine hematological investigations were advised, which were non-contributory. Serological tests for herpes simplex virus (HSV) and Mycoplasma Pneumonia were done, which were negative.
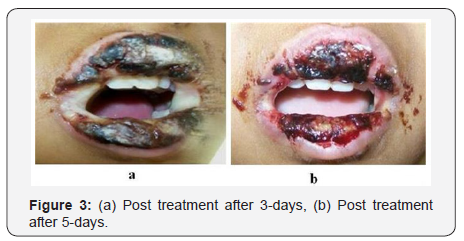
Treatment: The following medications were administered- Systemic corticosteroid (Prednisolone- 15mg/day in divided doses for 5 days), topical anesthetic and analgesic gel (Dologel) and 0.5% lacrimos eye drop. The dose of steroids was gradually tapered over next week. He responded well to the treatment and showed significant improvement after 3 days (Figure 3). After 10 days follow-up, there was a drastic change with resolution of the lesions (Figure 4).

Discussion
Steven Johnson Syndrome (SJS) is an immune-complex mediated hypersensitivity reaction. It was first reported in 1922 by pediatricians A.M. Steven and F.C. Johnson, as an acute mucocutaneous syndrome in two young boys [4,5], with manifestations of severe purulent conjunctivitis, stomatitis with extensive mucosal necrosis, and purpuric macules.
SJS is caused by many factors like drugs, viral infections (HSV and Mycoplasma Pneumonia), bacterial infections andmalignancies [5]. Most of the cases of SJS are drug induced and lethal. According to Patel PP et al (2012) [2] a study conducted on 1769 patients with ADRs only 3.33% (59 patients) were reported with SJS. Most common drugs causing SJS are antimicrobials (cephalosporin’s, quinolones, aminopencillins, tetracyclines, macrolides), anticonvulsants, aullopurinal, nevirapine, isotretinoin, antidepressants (mirtazapine), tumor necrosis factor-alpha (TNF-alpha) antagonists (Infliximab, etanercept, adalimumab), NSAIDs [5,6]. In our case the offending drug was penicillin.
SJS is a severe life threatening disease, which is sudden in onset associated with fever, myalgia, and arthalgia. Typically it manifests on the skin and mucous membranes with a clinical sign and symptoms of rashes, blisters or erosions on the skin covering less than 10% of the body’s surface area, with variable extent and consist of atypical maculopapular lesions of erythema multiforme (EM), bullous or rarely pustular lesions which progress to cause epithelial necrosis [7]. The oral cavity shows extensive bulla formation followed by erosions with characteristic hemorrhagic crustations on lips. SJS with minor presentations are seen involving eyes, nasal, gastrointestinal tract, respiratory tract and genital areas [5]. The clinical manifestation of eye involvement shows bulla formation, conjunctivitis, corneal ulcerations and panophthalmitis [7,8]. In the present case skin, eyes, genitals and oral cavity were involved, with maculopapular lesions on the skin and genitals, erythematous eyes with discharge and erosions involving oral cavity with hemorrhagic encrustations on the lips.
The diagnosis of SJS cannot be definitely established based on any specific laboratory tests. It is purely based on history and clinical features of the patient. But sometimes incisional biopsy and culture methods were performed to differentiate from other lesions like EM, herpes simplex infections, pemphigus, pemphigoid, subepithelial bullous dermatosis, bullous disease of childhood and linear IgA disease [5,9].
The management of patients with SJS is based on the etiological agents causing it, and treatment must be prompt with early recognition of the agents. Withdrawal of offending drug is essential in drug induced SJS, with specific treatment like symptomatic and supportive therapy are required for good prognosis and thus mortality rates are reduced according to SCORTEN criteria [5]. The supportive therapy like fluid replacement and electrolyte balance is given as in burns cases and symptomatic treatment like analgesic, topical antiseptics (0.5% silver nitrate or 0.05% chlorhexidine), topical anesthetics (5% xylocaine) and eye drops (0.5% carboxymethylcellulose sodium) are advised [5].
The management of SJS/TEN also requires a multidisciplinary team approach with various specialities like dermatologists, pediatricians, ophthalmologists, microbiologists, pathologists, nutritionists and general physician’s [10].
Conclusion
SJS is a severe mucocutaneous disease, mostly occurs by ADRs, majorly involving skin and oral cavity with manifestationsof blisters and erosions. As there remains no specific diagnostic test for SJS, early diagnosis based on history and clinical features of disease remains essential to promptly initiate appropriate management with withdrawal of the offending drug and proper follow up to reduce complications and mortality. So every clinician should be aware of the typical presentation of SJS.


Comments
Post a Comment