In vitro Comparison of Marginal Fit of Cad-Cam Zirconia, SMLS Co-Cr, Pressable Lithium Disilicate, and Cast Ni-Cr Copings - Juniper Publishers
JUNIPER
PUBLISHERS-OPEN ACCESS JOURNAL OF DENTISTRY & ORAL HEALTH
In vitro Comparison of Marginal Fit of Cad-Cam Zirconia, SMLS Co-Cr,
Pressable Lithium Disilicate, and Cast Ni-Cr Copings
Authored by Jitendra J Mete
Abstract
Context:Clinically acceptable
marginal fit of crowns has been the focus of various investigations.
There is limited literature comparing marginal accuracy CAD-CAM
zirconia, SMLS Co-Cr, Pressable Lithium Disilicate, and cast Ni-Cr
copings.
Aim:Evaluate and compare marginal accuracy of CAD-CAM zirconia, SMLS Co-Cr, Pressable lithium Disilicate, and cast Ni-Cr copings.
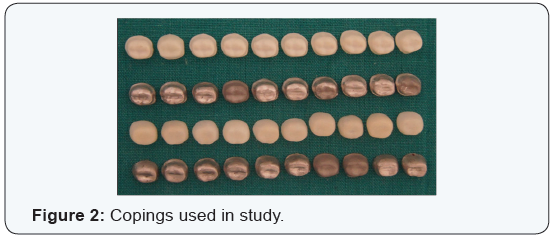
Methods and Material: Forty
copings were fabricated (Ten each in Group I - CAD- CAM zirconia, Group
II - SMLS Co-Cr, Group III - lithium disilicate, and Group IV- cast
Ni-Cr copings) on a standardized stainless steel model with long chamfer
finish line. Four areas around the tooth surface namely mesial (M),
distal (D), buccal (B) and lingual (L) surfaces were digitally analyzed
for marginal fit under the stereomicroscope.
Stastical Analysis: Comparison between groups was done by using one-way ANOVA test followed by a Post Hoc Tukey-Kramer multiple comparisons test.
Results: The mean marginal gap
(in μm) for Group I on lingual, buccal, mesial and distal surface was
37.05, 38.54, 37.61 and 36.09 respectively. The mean marginal gap (in
μm) of Group II on lingual, buccal, mesial and distal surface was 48.48,
50.88, 50.12, and 49.5 respectively. The mean marginal gap (in μm) of
Group III on lingual, buccal, mesial and distal surface was 63.04,
64.07, 64.97 and 65.81 respectively. The mean marginal gap (in μm) of
Group IV on lingual, buccal, mesial and distal surface was 75.68, 74.75,
73.86, and 72.78 respectively.
Conclusion: The marginal fit of
CAD-CAM zirconia copings is more accurate as compared to SMLS Co-Cr,
pressable lithium disilicate and cast Ni-Cr alloy copings on a
standardized metal model.
Keywords: Marginal Gap; Stereomicroscope; CAD – CAM; Metal Laser Sintering; Pressable CeramicAbbreviations: SMLS: Selective Metal Laser Sintering; Co-Cr: Cobalt-Chromium Alloy; CAD: Computer Aided Designing; CAM: Computer Aided Manufacturing; CNC: Computer Numerically Controlled (CNC); HIP: Hot Isostatic Pressing.
Introduction
The success of a dental restoration is determined by 3
main factors: esthetic value, resistance to fracture, and marginal
adaptation [1-5]. Inadequate marginal fit leads to cement dissolution,
plaque accumulation, which increases the risk of carious lesions &
periodontal diseases [6-11].
Traditionally metal copings have been fabricated by
the lost wax technique and casting method. Inaccurate marginal fit of
copings fabricated by this technique may result from contraction of
impression material, distortion of wax patterns, or irregularities in
the cast metal. Newly developed selective metal laser sintering (SMLS)
technique uses a high power laser to fuse the small particles of metal
into a mass that has a desired 3-dimensional shape. The laser
selectively fuses powdered material by scanning cross-sections generated
from the 3-dimensional digital description of the part (for example,
from a CAD file or scan data) on the surface of the powder bed. SMLS is a
CAD/CAM based technique in which frameworks and metal copings can be
designed and fabricated using cobalt-chromium alloy (Co-Cr). Co-Cr
powdered alloy used in this technique has slight variations in
composition. The molybdenum content in the alloy powder used in SMLS is
comparatively less than the alloy which is used for conventional
casting. After each cross section is scanned, the powder bed is lowered
by one-layer thickness and a new layer of material is applied on top.
The process is repeated until the part is completed. Advantage of SMLS
system include easy fabrication of complicated shapes and short working
time due to elimination of the procedures of fabricating a wax pattern,
investing, burning and casting works [12].
Development in ceramic materials such as lithium disilicate,
and zirconium oxide cores, uses of hot press and CAD-CAM
equipment have opened up new path for all ceramic restorations
[13]. CAD-CAM not only provides reproducible results fulfilling
certain standards but also reduces the errors arising from the
technicians. However, it is associated with higher cost. When
measuring the marginal gap after cementation, the same number
of teeth or steel dies as that of restoration sample is needed to
control the variables. On the other hand, only one tooth or steel
die is needed if the measurement is done without a luting agent.
Investigators have found a significant increase in the marginal
discrepancy after cementation [14,15]. These results, however,
varied according to the luting agent. The marginal fit was,
therefore, measured without cementation for variable control in
this study.
There is limited literature which compares marginal accuracy
of CAD-CAM zirconia, SMLS Co-Cr, Pressable lithium disilicate, and
cast Ni-Cr copings. So the present in vitro study was conducted to
evaluate and compare the marginal accuracy of CAD-CAM zirconia,
SMLS Co-Cr, Pressable lithium disilicate, and cast Ni-Cr copings.
Methods and Material
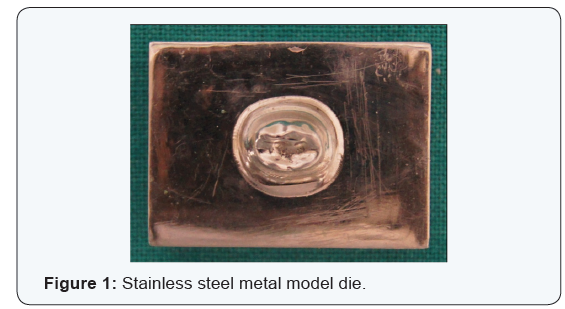
Fabrication of stainless steel master model
For fabricating a standardized master model, a typhodont
mandibular first molar tooth was first scanned using threedimensional
(3-D) computer-aided designing (CAD) software. After
scanning of the mandibular first molar tooth, a uniform chamfer
finish line of 1.2 mm in width, 6-degrees occlusal convergence, 1.5
mm reduction on functional cusps with functional cusp bevel and
1 mm reduction on non-functional cusps simulating a prepared
mandibular first molar was carried out on the CAD software. A
rectangular platform measuring 4 cm in length, 3 cm in breadth
and base of thickness 2 cm made of stainless steel material was
chosen for the purpose of milling. To fabricate a standardized
master model consisting of a metal die exactly in the centre of the
rectangular platform, computer-aided manufacturing (CAM) was
carried out using the data obtained from the CAD software which
was then transferred to the computer numerically controlled
(CNC) milling machine (LAVA CNC 500) and engraving was done.
After engraving, finishing and polishing of the master model was
carried out. The stainless steel metal master model was used to
fabricate all the copings and also to serve as an abutment for the
measurement of marginal discrepancy.
Fabrication of CAD-CAM zirconia copings
A dental CAD/CAM system, 3M LAVA CAD/CAM system (3M
ESPE Dental Products St. Paul, MN U.S.A) was used to fabricate
the 10 zirconia copings used in this study. Metal model of the
abutment was scanned using 3M Scanner. Scanned data were then
converted into CAD data. Copings for all-ceramic crowns were
designed using the dental wings supported by 3M software. No
cement space was included for the margin, and 45 μm was used for
the axial and occlusal surfaces of the abutment. Thickness of the copings were designed to be 0.5 mm. Design data were converted
into processing data and sent to the processing machine (CNC 500
LAVA 3M).The zirconia blocks were cut and milled, and then the
milled blocks were finally sintered to make zirconia copings. The
internal surfaces & margins of the copings after placing on die
were examined using a binocular loupe (HEINE HR-C 2.5x, HEINE,
Herrsching, Germany) to check the complete seating.
Fabrication of Pressable lithium disilicate copings
Ten copings were fabricated from lithium disilicate glass
ceramics (IPS e.max Press, Ivoclar Vivadent AG) using a
combination of the lost-wax and heat-press techniques. Die
lubricant (Isocera, Bego, Germany) was applied to the metal die.
Wax patterns were fabricated on the dies using dip wax technique
to form wax copings. The patterns were contoured parallel to
the emergence profile and margins were manually sealed under
1.5×magnification.The thickness of the copings was confirmed
with a thickness gauge (POCO 2N; Kroeplin, Schluchtern, Germany)
to be 0.5mm. Finally, to re-adapt the margin, the pattern was
reflowed completely through the wax over a band approximately
1mm wide with a well heated instrument, PKT No.1. Wax was then
added to fill the depression, and when the pattern had cooled,
the marginal excess was carved and the margin was burnished.
Patterns were invested in phosphate bonded investment (IPS
Press VEST Speed, Ivoclar Vivadent AG). After wax elimination
glass ceramic ingots (HO 2, Ivoclar Vivadent AG) were plasticized
at 9300C and vacuum pressed (EP 500 press furnace, Ivoclar
Vivadent AG) into an investment mold. After a holding time
of 25 min the pressed crowns were divested, separated and
cleaned by applying 1% hydrofluoric acid (IPS e.max Press Invex
Liquid, Ivoclar Vivadent AG) for 10 min. Internal surfaces were
sandblasted with 100 μm aluminum oxide at 2 bar pressure. The
internal surfaces of the copings were examined using a binocular
loupe (HEINE HR-C 2.5x, HEINE, Herrsching, Germany) and any
visible metal nodules were removed with water cooled diamond
bur. To detect the invisible nodules or irregularities, the internal
surfaces of the copings was checked on the master dies using vinyl
poly-siloxane disclosing paste (Fit checker; GC Corporation). After
removing the copings from the die, the contact spot, marked bythe indicator on the inside of the copings was examined visually
using a binocular loupe (HEINE HR-C 2.5x, HEINE, Herrsching,
Germany), these marked spots were removed until no internal
binding was occurred and a uniform thickness of disclosing
paste achieved. Finally, the copings were fitted to metal die. All
copings were manufactured under supervision by the same dental
technician.
Fabrication of cast Ni-Cr alloy copings
For making nickel-chromium (Ni-Cr) alloy copings, wax
patterns were fabricated in similar way as for Pressable lithium
disilicate copings. The wax patterns were invested with a
phosphate-bonded investment (Bellabond Plus, Bego, Germany)
and cast with Ni-Cr (Bellasun, Bego, Germany) alloy using an
induction casting machine (LC Cast – 60, Confident equipments).
After casting, the ring was bench cooled to room temperature and
divested. The copings were sandblasted with 50-μm Al2O3 at 0.2-
MPa air pressure to remove the investment. The internal surfaces
of the copings were examined using a binocular loupe (HEINE HR-C
2.5x, HEINE, Herrsching, Germany) and any visible metal nodules
were removed with a tungsten carbide bur (No. H71EF; Brasseler
GmbH and Go KG). To detect the invisible nodules or irregularities,
the internal surfaces of the copings was checked on the master
dies using vinyl poly-siloxane disclosing paste (Fit checker; GC
Corporation). After removing the crown from the die, the contact
spot, marked by the indicator on the inside of the copings was
examined visually using a binocular loupe (HEINE HR-C 2.5x,
HEINE, Herrsching, Germany), these marked spots were removed
until no internal binding was occurred and a uniform thickness of
disclosing paste achieved. Finally, the restorations were fitted to
metal die. All copings were manufactured under supervision by
the same dental technician.
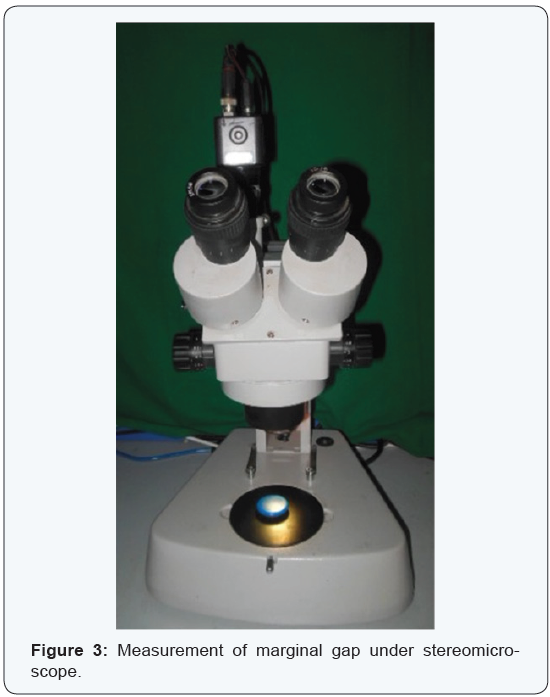
Every finished coping was placed on the prepared metal die
and checked for complete seating after which it is evaluated for
the marginal fit accuracy using a stereomicroscope (Wuzhou
New Found Instrument Co. Ltd., China, Model Xtl 3400 E). During
stereomicroscope evaluation copings were secured to master
die model using vice holder. Stereomicroscopic images were
analyzed using image analysis system (Chroma Systems Pvt. Ltd.
India) and measurements for marginal gap were taken on deepest
portion of copings on lingual, buccal, mesial and distal. Total
160 measurements were recorded of 40 copings, 10 of each four
study groups. The mean and standard deviation of marginal gap
of four Groups on lingual, buccal, mesial and distal surface was
calculated. Tukey-Kramer multiple comparison test was applied
for comparative evaluation of marginal fit in different groups.
Results
The mean ± SD marginal gap of Group I on lingual, buccal,
mesial and distal surface was 37.05 ± 4.19, 38.54 ± 3.68, 37.61 ±
4.05 and 36.09 ± 4.18 respectively. The mean ± SD marginal gap
of Group II on lingual, buccal, mesial and distal surface was 48.48
± 5.99, 50.88 ± 6.0, 50.12 ± 5.91 and 49.5 ± 5.67 respectively. The
mean ± SD marginal gap of Group III on lingual, buccal, mesial and
distal surface was 63.04 ± 4.21, 64.07 ± 4.26, 64.97 ± 4.41 and
65.81 ± 4.49 respectively. The mean ± SD marginal gap of Group
IV on lingual, buccal, mesial and distal surface was 75.68 ± 10.38,
74.75 ± 10.68, 73.86 ± 10.71 and 72.78 ± 10.61 respectively.

Tukey-Kramer multiple comparison tests was applied for
comparative evaluation of marginal fit in different groups. The
marginal fit of Group I on lingual, buccal, mesial, and distal
surfaces as compared to Group II, Group III and Group IV was
found to be statistically significant (p<0.001) (Table 1) & (Figures
1-3). The marginal fit of Group II on lingual, buccal, mesial, and
distal surfaces as compared to Group III and Group IV was found
to be statistically significant (p<0.001).The marginal fit of Group
III on lingual, buccal, and mesial surfaces as compared to Group IV
was found to be statistically significant (p<0.001).The marginal fit
of Group III on distal surface as compared to Group IV was found
to be statistically not significant (p>0.05).
Discussion
The ultimate goal of successful fixed partial denture (FPD)
prosthesis can be achieved only when an accurate and precise
marginal fit is produced. Microleakage and marginal openings are
important causes of fixed restoration failures. One of the reasons
for high microleakage is the amount of marginal gap, the increase
of which causes greater microleakage, because the amount of
cement exposed to oral fluids depend on the extent of the marginal
gap [16].
Marginal discrepancies in the range of 40-120 μm have been
reported to be clinically acceptable with regard to longevity
of a restoration [17]. All the copings tested in this study are in
the range of 35-80 μm, which is within acceptable limits. The
different materials and applied techniques in the manufacturing
of crown systems have significant effects on the strength of the
final restoration as well as the marginal fit. Imperfect restoration
margins offer recesses for adherence of oral bacteria, which may
cause secondary caries and traumatic gingival irritation [18]. This
in vitro study examined the marginal adaptation of four types of
copings, consisting of frameworks fabricated using CAD/CAM
zirconia, selective metal laser sintering (SMLS), pressable lithium
disilicate and cast nickel-chromium (Ni-Cr) alloy. The marginal
discrepancies of group CAD/CAM zirconia were significantly
smaller compared to those of the other three study groups.
A stainless steel die was used for making copings and served
as the abutment for the measurement of marginal discrepancy for
all the copings made in this study. The advantages of the stainless
steel die are standardized preparation and avoidance of wear of
the die during the coping fabrication and measurements. The deep
chamfer finish line preparation was selected because it meets
the requirements for all the four study groups used in this study
[19]. The majority of marginal discrepancy is known to develop
during the oxidation cycle for metal copings [20]. This is often attributed to the release of residual stresses incurred during
casting, grinding or polishing phases of the procedure. As the
prostheses cools from the firing temperature, the difference in
thermal contraction between the metal coping and the porcelain
may result in additional marginal discrepancy [21].
The mean marginal gap widths of the CAD/CAM zirconia
fabricated superstructures were significantly smaller than those of
the selective metal laser sintered frameworks. This finding can be
attributed to advancements in scanning technology, restorationdesigning
software with improved margin detection and precision
milling technologies. The vertical marginal gap values obtained
were within the range of clinical acceptance i.e. 40 μm to 120
μm. The CAD/CAM zirconia system mills the framework with the
final dimensions out of a densely sintered Y-TZP (Yittria stabilized
Tetragonal Zirconia Polycrystals) blank which is fabricated with
the ‘Hot Isostatic Pressing (HIP)’ technology. This technology
involves sintering partially sintered zirconia material at a high
temperature in a high density, homogenous zirconia material
with improved mechanical properties [22]. For CAD/CAM ceramic
crowns, marginal gaps of 17 μm to 118 μm have been reported by
various authors [23]. Similar results were obtained in the present
study.
However, a higher accuracy was achieved with the soft,
partially sintered Y-TZP ceramics compared with the hot isostatic
pressed (HIP) Y-TZP blocks. This finding can be attributed to the
ease of machining and the precisely controlled sintering cycle in
a specially designed sintering oven which aided in achieving a
consistently accurate fit. The lesser accuracy of hard HIP-YTZP
ceramics can be attributed to their extreme hardness and higher
flexural strength (> 1,200 MPa), which can cause greater wear of
the milling burs and a reduction in the efficiency of the milling
unit consequently leading to lesser accuracy of fit. The Post Hoc
comparison of both hard and soft types of ceramics showed no
statistical significance, indicating that either form of Y-TZP ceramic
produces clinically acceptable restorations. The comparable
mechanical properties and the relative ease and speed of soft
Y-TZP blank milling may explain why more operators choose this
method to fabricate zirconia restorations, whereas only a small
number prefer the hard Y-TZP blanks [24].
The results of the present study suggest that the new
zirconia
ceramic systems fabricated with CAD/CAM technology presents
better marginal fit as compared to selective metal laser sintered
copings. These results were in accordance with a study conducted
by Ece Tamac et al. [25]. The results of this study shows that
selective metal laser sintered copings shows better marginal fit
than pressable lithium disilicate and cast Ni-Cr alloy copings. This
finding can be attributed to the fact that additive manufacturing
is used during selective metal laser sintered copings fabrication
and this technique uses a high power laser to fuse small particles
of metal into a mass that has a desired 3-dimensional shape. The
laser selectively fuses powdered material by scanning crosssections
generated from a 3-dimensional digital description of
the part (for example from a CAD file or scan data) on the surface of a
powder bed. After each cross-section is scanned, the powder
bed is lowered by one-layer thickness, a new layer of material
is applied on top and the process is repeated until the part is
completed. These results are in accordance with Montero J. et
al who concluded that selective metal laser sintering may be an
alternative to vacuum-casting of base metals to obtain passivefitting
implant-supported crown copings [26].
Glass-ceramics have superior stability, biocompatibility,
esthetics, and chemical inertness, making them a viable
alternative restorative material. Leucite-reinforced glass-ceramics
were originally designed for CAD/CAM restorations because of
their high durability and ability to be milled accurately. These
ceramics are reinforced by the incorporation of leucite crystals
into their structure, giving them improved toughness and strength
[27]. In the present study, the leucite-reinforced glass-ceramic
superstructures showed higher accuracy of marginal fit compared
with the cast Ni-Cr superstructures.
IPS Empress Copings show less marginal gap than the
conventionally casted Ni-Cr alloy copings. IPS Empress 2 (Ivoclar
Vivadent, Schaan, Liechtenstein) is a lithium-disilicate glass
ceramic (SiO2-Li2O) that is fabricated through a combination of
the lost-wax and heat-pressed techniques. A glass-ceramic ingot
of the desired shade is plasticized at 920°C and pressed into an
investment mold under vacuum and pressure. Its predecessor,
IPS Empress (Ivoclar Vivadent) is a leucite-reinforced glass
ceramic (SiO2-Al2O3-K2O) which, due to its strength is limited in
use to single unit complete-coverage restorations in the anterior
segment. IPS Empress 2 has improved flexural strength by a
factor of 3 over IPS Empress, can be used for 3-unit fixed partial
dentures in the anterior area and can extend to the second
premolar. The framework is veneered with fluoroapatite-based
veneering porcelain (IPS Eris; Ivoclar Vivadent), resulting in a
semi translucent restoration with enhanced light transmission.
IPS e.max press (Ivoclar Vivadent) was introduced in 2005 as an
improved press-ceramic material compared to IPS Empress 2.
It also consists of a lithium-disilicate pressed glass ceramic, but
its physical properties and translucency are improved through
a different firing process [28]. Yeo IS et al. [29] concluded that
the IPS Empress 2 systems showed the smallest and most
homogeneous gap dimension, whereas the conventional In-Ceram
system presented the largest and more variable gap dimensions
compared with the metal ceramic restorations.
The conventionally casted Ni-Cr superstructures show more
marginal gap when compared with the CAD/CAM superstructures.
This finding can be attributed to the expansion and contraction
associated with the impression materials, gypsum, wax pattern
distortion during removal and the spruing process are other factors
that may affect the accuracy of superstructures fabricated using
the lost-wax process [30]. These results are in accordance with
a study conducted by Tamer E. Shokry et al. [31] who concluded
that titanium copings fabricated by CAD/CAM demonstrated the
least marginal discrepancy among all groups, while the base metal
(Ni-Cr) groups exhibited the most discrepancy of all groups tested.
It is difficult to interpret the statistical results of the previous
studies because of variations in sample size, the measurement
per specimen and the measurement methods used. There is
no standardized method to measure the marginal fit. The most
common methods are ‘direct viewing, sectioning, probing and
explorative and visual examinations’ [32]. In the current study,
the direct viewing of the crown on a die is used to measure the
marginal fit of all the copings. Direct viewing has the advantage of
being nondestructive and therefore applicable to clinical practice.
The vertical cervical marginal gap measurement was selected
as the most frequently used to quantify the accuracy of fit of a
restoration [33].
Conclusion
Within the limitations of the present study, following
conclusions can be drawn:
- The marginal fit of CAD/CAM zirconia copings is more accurate as compared to selective metal laser sintered (SMLS), pressable lithium disilicate and cast Ni-Cr alloy copings on a standardized metal master model.
- Base metal alloy (Ni-Cr) exhibited a discrepancy that was significantly higher than the rest of the groups.
- The marginal discrepancies of all the copings were within the clinically acceptable range of 80-120 μm.
For more Open Access Journals in Juniper Publishers please
click on: https://juniperpublishers.com
For more articles
in Open Access Journal of Dentistry & Oral Health please click on:

Comments
Post a Comment