The Relationship Between Resonance Frequency Analysis (RFA) and Insertion Torque of Dental Implants: an in Vitro Study- Juniper Publishers
Juniper Publishers-Open Access Journal of Advances in
Dentistry & Oral Health
Abstract
Purpose: The aims of the present
study are to correlate the ISQ values, registered by the Osstell ISQ
system, with the insertion torque during the placement of the implant,
and to assess the influence of the thread initiator on the ISQ values
and on the insertion torque.
Materials and methods: 140 rough
surface implants screw-shaped implants, placed in 10 bovine ribs, were
assigned to Group A (using the thread initiator before the insertion of
the implant) or Group B (thread initiator was not used). The implants
were implantedusing a manual torque wrench so insertion torque was
registered. Once the implants were in place, primary stability was
measured by means of RFA with the Osstell ISQ.
Results: When the thread initiator
was used (group A), the mean insertion torque was 24,36 ± 14,88 N and
when the thread initiator was not used (group B) the mean insertion
torque was 35,30 ± 10,51N. The mean ISQ of the thread initiator group
was 69,14 ± 8,39 and of the non thread initiator group was 72,17 ± 5,76.
Pearson’s correlation coefficient was 0,587 (p<0,05) for group A and
0,193 (p<0,11) for group B.
Conclusions: It seems that the fact
of using or not the thread initiator have no influence in the ISQ
values. However, the IT decreased when the thread initiator is employed.
Keywords: Implant stability, Insertion torque, ISQ, Osstell, osseointegrationIntroduction
Implant stability depends directly on the mechanical
connection between the implant surface and the surrounding bone. Initial
stability, a consequence of an immediate mechanical adaption between
the implant and the bone site, depends on the density of the bone tissue
(the bone quantity and quality), the surgical technique used and the
congruity of the site and macrostructure of the implant [1-6]. Secondary
stability is the result after the formation of woven and lamellar bone
around the dental implant surface as a secondary bone contact [2,3].
Primary stability was always considered a fundamental prerequisite to
acquiring osteointegration [3,7] and it is now even more important,
whenever clinicians want to use immediate loading protocols [8,9].
Extensive micromotion during healing and functional loading is one
likely reason for implant failure as this may result in
non-physiological conditions for bone formation and remodelling [10].
The greater the primary stability, the smaller the micromotions are
between implant and bone. The micromotion promotes the formation of a
soft tissue capsule around the implant, and as a result implant failure
may occur [11,12].
Various non-invasive stability measurement techniques
(i.e. methods of percussion, radiography, resonance frequency analysis,
placement resistance, reverse torque and vibration
in the sonic and ultrasonic ranges) were used to measure the
stability of endosseous dental implants [2,3,5,13]. One of the
quantitative methods is the insertion torque (IT) [3]. The IT,
was described by Johansson and Strid [14,15], is the moment of
force necessary to seat the implant into the osteotomy site, and it
furnishes worthy information about the quality of the local bone
[1- 5,16]. The determination of the IT is done by a torque gauge
incorporated within the drilling unit or with a torque wrench
during the insertion of the implant [8,9]. It is an easy method,
but it can be measured only once, at the time of the insertion of
the implant. It is not used to monitor the stability over time.
Resonance frequency analysis (RFA) was introduced by
Meredith in 1996 [6,17]. It is a non-invasive, reliable, and objective
method where the device measures the degree of implant stability
at any time during the course of implant treatment and loading
[3, 5,18,19]. The technique has been demonstrated to evaluate
implant stability as a function of interface stiffness [6,15,20].
Although there is some controversy about it, a recent study has
demonstrated a correlation between bone density and ISQ and
displacement measurements. Thus, clinical measurements of
implant micromotion would be one way to identify implants at
risk of failure [21]. The implant/bone interface is measured from
RFA as a reaction to oscillations exerted onto the implant ⁄ bone
contact, where the unit of measurement is recorded as implant
stability quotient (ISQ). RFA is assessed by the instrument
Osstell (Osstell AB, Göteborg, Sweden). Osstellgives the ISQ on
a scale from 1 to 100. The higher the ISQ number, the higher the
stability [22,23].
Clinically, ISQ values have been correlated with changes
in implant stability during osseous healing. Thus, IT and ISQ
values are thought to have a positive correlation. However, the
correlation of higher IT torque translating into higher primary
stability may not always be true because the quantity and quality
of bone varies significantly among patients [4].
The aims of the present study are to correlate the ISQ values,
registered by the Osstell ISQ system, with the insertion torque
during the placement of the implant and to assess the influence
of the thread initiator on the ISQ values and on the insertion
torque.
Material and Method
140 rough surface implants (Shot Blasting®: alumina particle
sandblasting and acid passivation) screw-shaped implants
(Essential® Cone, Klockner Implant System, SOADCO, Andorra)
were used. All implants had a diameter of 4mm (diameter at
platform level is 4,5mm), a length of 10mm and a mechanized
collar height of 1,5mm. The implants were assigned to one of the
following groups:
a) Group A:complete drilling sequence, following the
manufacturer’s protocol and using the thread initiator before the
insertion of the implant.
b) Group B:complete drilling sequence without using the
thread initiator.
The implants were placed in 10 bovine ribs (bone quality
type II, according to Leckholm & Zarb [24], by an experienced
clinician (user and knower of the Klockner Implant System for
more than 2 years), following the manufacturer’s protocol. 14
implants were place in each rib. The osteotomy was performed
under abundant irrigation with sterile saline solution at 800
rpm. The implants were inserted using a manual torque wrench
so that the rough/smooth interface was placed at bone crest
level. The distance between the implants had to be at least 10mm
in between of the centre of the implants. As the implants were
place with manual torque wrench, the exactly insertion torque
was registered.
Once the implants were in place, primary stability was
measured by means of RFA with the Osstell ISQ, by a second
experienced clinician in the use of the ISQ device. The ISQ was
measured over the Smartpeg screwed directly to the implant
by the specific plastic hand-screwdriver. One Smartpeg is
used every 5 implants (so 10 measurements were made with
each transducer). The ISQ was registered perpendicular to the
Smartpeg in 2 different positions:
- The ISQ is registered from the front of the rib; and
- The stability is registered from the right of the rib (90º from the first measurement). At each position, the ISQ was registered once.
SPSS 19.0 software (SPSS, Chicago, IL) was used for the
statistical analysis. Mean values and standard deviations and
the Pearson Correlation Coefficient were calculated. The normal
distribution of the values and the homogeneity of the variances
were tested through a Kolmogorov-Smirnov test. The differences
between the mean values were compared with the nonparametric
Mann-Whitney test. Then, all the values were grouped
according to the ISQ and IT registrations and the differences were
compared with the non-parametric Kruskal-Wallis test.When
significant differences were obtained, 95% confidence intervals
were found for average and mean differences (p < 0.05).
Results
When the thread initiator was used (group A), the mean
insertion torque was 24,36 ± 14,88N and when the thread
initiator was not used (group B) the mean insertion torque was
35,30 ± 10,51N. The mean ISQ of the thread initiator group was
69,14 ± 8,39 and of the non thread initiator group was 72,17 ±
5,76. Pearson’s correlation coefficient was 0,587 (p<0,05) for
group A and 0,193 (p<0,11) for group B.
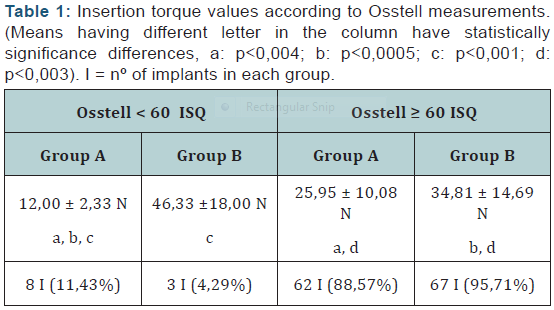
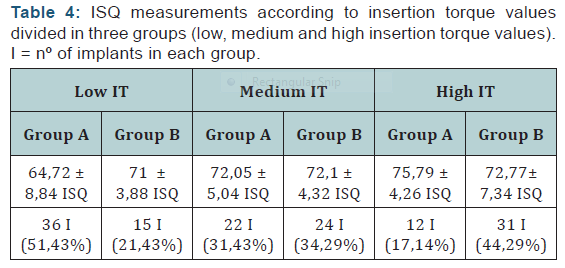
The mean insertion torque values according to the ISQ
was studied in Table 1. Statistically significant differences were
found between group A when the ISQ was < 60 and ≥ 60; between
group A when the ISQ was < 60 and group B when the ISQ was ≥
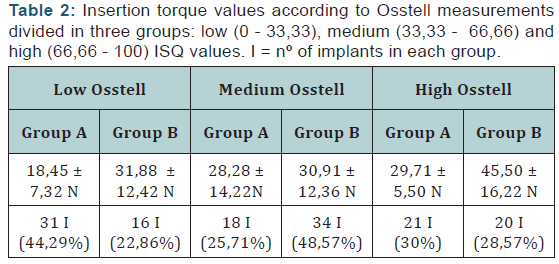
60 and between group A and B when the ISQ was <60 and when the ISQ was ≥ 60 (shown in Table as a, b, c and d). In Table 2 the
insertion torque related to the ISQ divided in three groups (low,
medium and high ISQ values) was showed.
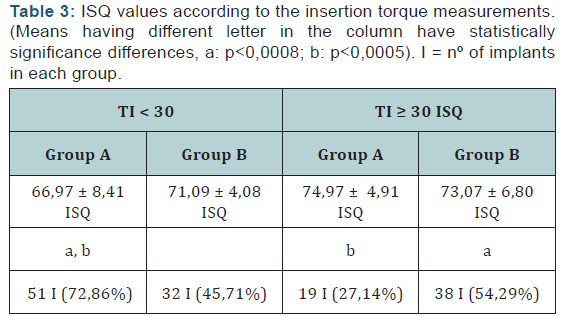
The mean ISQ values related to the insertion torque are given
in Table 3. Statistically significant differences were only found
between group A when the IT was < 30 N and ≥ 30 N and between
group A when the IT was < 30 N and group B when the IT was ≥
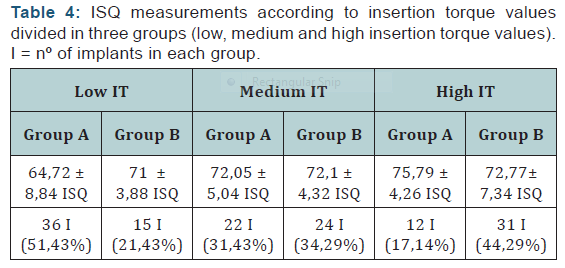
30 N (shown in table as a, b). In Table 4 the ISQ values according
to the insertion torque divided in three groups (low, medium and
high IT) was showed.
Discussion
This study was conducted to evaluate the correlation
between the IT and the ISQ values obtained from the RFA. The
bone in which the implants are place is type II, according to
Leckholm & Zarb’s [24] classification. The mean ISQ in our study
was 69,14 ± 8,39 for the thread initiator group and 72,7 ± 5,76 for
the non thread initiator group. These results are similar to those
of other trials examining the ISQ in cow ribs (also bone quality
type II). In 2009, Andrés-García et al. [25] found a mean ISQ of
70,86 ± 3.4 and 70 ± 3,8 when placing two different implants
(3,7 x 10mm Zimmer® Dental and 4x 10 mm Nobel Biocare®)
in cow ribs with bone quality type II-III. In 2014, Romanos et al.
[26] analysed the ISQ of three types of implants (two types of
straight-screw type implants -one with polished collar and the
other one without- and one tapered-screw type implant) placed
in cow ribs, bone quality type III. The implants were Straumann,
length 10 mm and diameter 3,3 mm. The mean ISQ values were
75,02 ± 3,65, 75,98 ± 3,00 and 79,83 ± 1,85, respectively. The
slight differences between the results of those trials and the
present one could be due to the different macro design of the
implants used. The literature agrees that the most appropriate
design is endosseous screw-shaped implants.
Pearson’s correlation coefficient showed that the correlation
between the IT and the RFA is positive: 0,587 (p<0,05) for group
A and 0,193 (p<0,11) for group B. The correlation for the group
B is very low. This means that when the thread initiator was
used there were more correlation in between the two variables
and that when thread initiator is not used there was almost no
correlation between them.
The data published about this theme is contradictory. Data
presented by Turkyilmaz et al. [3] in 2006, is in contrast with
the results of group B of the present study. They analysed 142
Brånemark implants and reported an Spearman correlation of
0,583 that is very far from 0,193 reported for group B, but is
similar to the correlation reported for group A. The reason for
this difference appears unclear, but it could be explained by the
different design of the implants studied, as well as the smaller
number of the sample. Kahraman et al. [2], in 2009, found a
positive significant correlations between the IT and ISQ values at
the surgery (r = 0,78, p < 0,001), and at the prosthesis delivery (r
= 0,46, p < 0,01) when 16 Straumann Standard Plus Implants and
26 MIS Seven Implant were inserted in 13 patients. In 2010, Degidi
et al. [8] also reported a positive but low correlation between
IT and ISQ of 0,247 when 514 Xive Implants was inserted in 52
patients. Makari et al. [6] in 2012 showed a positive correlation
between IT and ISQ at baseline (r= 0,313, p< 0,049), at 3 weeks (r
= 0,472, p < 0,002), and at 6 weeks (r = 0,419, p < 0,007). In 2012,
Degidi et al. [9] published another study in which IT and ISQ was
evaluated in 4135 XiVE implants (Dentsply Friadent) inserted in
1045 patients. The correlation between the two variables in that
study was r = 0,218 (p < 0,0001). Also in 2012 Park et al. [13], viewed a correlation between the ISQ value and the maximum
IT value at the initial implant surgery (p < 0,01, r = 0,427); when
81 implants (Branemark with the external connection and ITI
implants with internal connection) were inserted in 41 patients.
They also found that Implants in the mandible showed higher
ISQ values than did those in the maxilla (p < 0,01), and ISQ values
were higher for the external type of implants compared to those
of the internal type (p < 0,01). As the implant diameter increased,
the ISQ value also increased (p < 0,01). Respect to the IT, they
showed that Implants in the mandible showed higher maximum
IT values than did those in the maxilla (p < 0,01), while male
patients exhibited higher maximum IT values than did females
(p < 0,01). Maximum IT values were higher with the external
implant type compared to those of the internal type (p < 0,01).
It is also suggested that ISQ and IT values are also dependent
on the system used [27,28], and self-tapping tapered implant
design brings higher initial stability than parallel wall cylindrical
implant systems [29]. O’Sullivan et al. [27] presented that
surface geometry had a great importance, in which the design
of the implant had the ability to increase the interfacial stiffness
at the implant ⁄ bone interface analysed by IT and RFA analysis.
When the IT and RFA are analysed by groups, our results are
in agreement with those of Degidi et al. [8]. It seemed that ISQ
values were generally high or medium, while low ISQ values were
quite rare. On the other hand, the distribution of IT values was
much more uniform between the groups. These data suggests
that RFA and IT represent two different features of primary
stability, with the first indicating the resistance to bending load
and the latter indicating the resistance to shear forces [8,30].
Conclusions
The fact of using or not the thread initiator has no influence
in the ISQ values. However, the IT decreased when the thread
initiator is employed.
Acknowlegement
The authors are grateful to Spanish Goverment for the CICYT
MAT-2015-67183-R
(MINECO/DEFDER,UE).
For more Open Access Journals in Juniper Publishers please click on: https://juniperpublishers.com
For more articles in Open Access Journal of Dentistry & Oral Health please click on:


Comments
Post a Comment