3D Printing Role in Oral and Maxillofacial Surgery Current and Future Trend- Juniper Publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF DENTISTRY & ORAL HEALTH
Abstract
The application of three-dimensional (3D)
printing enables virtual simulation surgery with tremendous details.
Data is usually obtained from detailed computed tomography (CT) scan and
the creation of material objects from digital images by depositing
layers into 3D structures. That can be used for training, education,
surgical planning and prosthetic reconstruction. We report on two
patients with complex reconstructive option in maxillofacial surgery
where 3D technology was utilized to analyze the tumor size, location,
and extension more precisely which drastically aids in better
preoperative planning Another case was for fabrication of custom 3D pure
titanium TMJ joint for reconstruction with optimal fit and function.
Keywords: 3D Printing;
Personalized medicine; Personalized surgery; Virtual surgery; Customized
prosthesis; Medical models; Custom TMJ; Titanium TMJ implant;
SclerodermaIntroduction
Medical applications for 3-D printing are expanding
rapidly and are expected to revolutionize health care. 3-D printing is
currently $700 million industry with only 11 million (1.6%) being
invested in medical applications. In the next 10 years it is expected
that 3-D printing will grow to $8.9 billion industry and 1.9 (26%)
billion is projected to be spend in medical applications.
Medical uses for 3-D printing can be categorized into three segments.
- Bioprinting tissue and organ;
- Creation of customized prosthetics, implantable devices and medical models
- Pharmaceutical drug dosage forms delivery and discovery.
Most reconstructive surgeons are familiar with
Charles Hull invention of 3-D printing “stereo lithography” in the early
1980’s. 3-D printing has since evolved and been applied in medicine
since the early 2000s. The first applications were used in dental
implants and custom prosthetic devices. Since then it’s applications
have significantly grown and most recent published reviews describe the
use of 3-D printing to produce bone, ears, trachea, blood vessels,
tissue organs as well as novel dosage form for pharmaceuticals by
personalizing drug printing fabrication at point of care while taking
into account patient age, gender, race and clinic response.
In this article we will focus on creation of
customize prosthesis, implantable devices and anatomical models within
the oral maxillofacial surgery practice [1].
Case 1 - Custom 3D pure titanium TMJ prosthesis
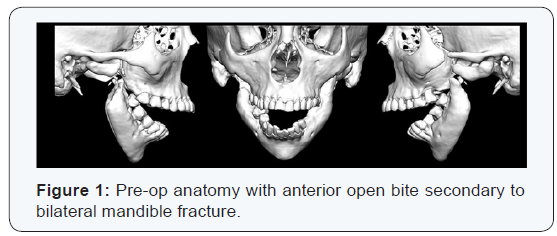
64 year old female with history of scleroderma has developed
a spontaneous pathologic fracture of her mandibular angle
bilaterally over 3 years ago. As a result, she developed significant
anterior open bite (Figure 1) with inability to chew food
requiring parental feeding for nutrition. She has seen multiple
surgeons within the US who have not been able to assist her
in her reconstructive needs due to the complexity and surgical
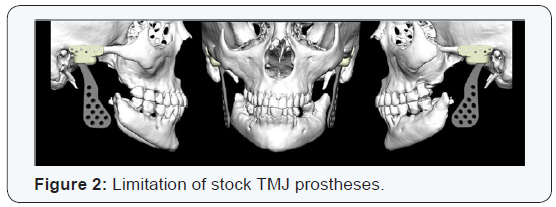
limitations. After CT evaluation and virtually ideal occlusion
alignment patient seem to have had significant bone resorption
bilaterally. Patient also does not have enough proximal condylar
head to allow any fixation. Additionally, a stock Total TMJ
prosthesis would not be able to reach the distal segment of the
mandible bilaterally after it is properly alignment (Figure 2). The
only option left is to create custom 3D temporomandibular joint
replacement pure titanium, as she exhibited sensitivity to nickel
(Figure 3). Currently Biomet custom joint are not FDA approved
in the United States however though the compassionate use
program we have been able to secure approval from the FDA
to custom make the implant to this the patient. Without the 3D
printing option for the custom prostheses this patient would
continue to suffer and live a life with significant compromised
quality of life [2].
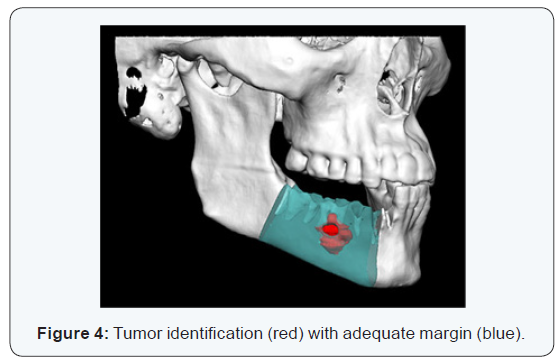
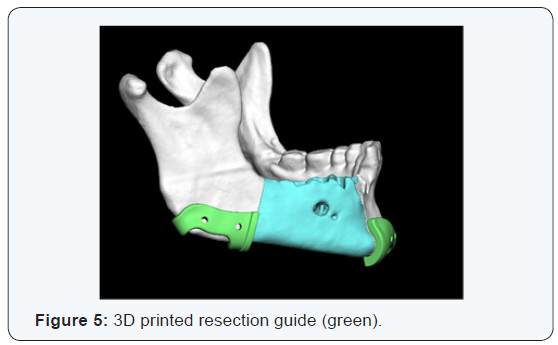
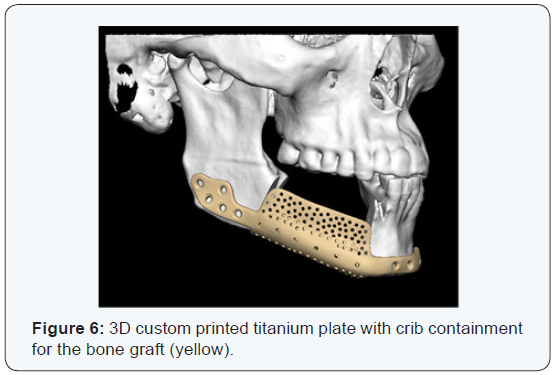
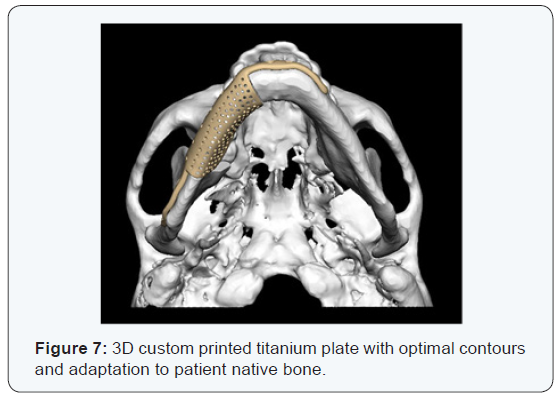
Case 2- Custom 3D Titanium Crib
34 year old male with destructive lesion in mandible that
was identified as a myxoma after biopsy of his right mandible.
Surgical plan was made to undergo partial mandibulectomy
with adequate margin. After conversation with the patient
we decided to reconstruct with custom 3D printing titanium
plate with crib containment. This allows for corticocancellous
bone graft from anterior iliac crest with bone marrow aspirate
concentrate (BMAC) and platelet rich plasma (PRP). BMAC is
a minimally invasive procedure used to collect bone marrow
from the patient’s own body (autologous) and concentrates it
to the optimal level while keeping all cell types, including adult
stem cells, mesenchymal cells and bone morphogenic protein
signal. While PRP acts are a stimulator for bone and soft tissue
healing via several growth factures enhancing bone maturity
and consolidation [3]. This 3D plate allows the patient to obtain
optimal cosmetic outcome as we are able mimic the pre-existing
contours, width and height of bone making dental implant
rehabilitation easier and more predictable (Figure 4-7).
Conclusion
Despite advances 3-D printing there are significant barriers
and controversies. Some of which are unrealistic expectation in
particularly regarding tissue/organ printed, safety and security
issues, and regulatory approvals. Regardless of the challenges
3-D printing is expected to play an important role in the trend
towards personalized medicine and revolutionize healthcare. It
is through the vision and collaborative support that allows us to
service these complex cases.
For more Open
Access Journals in Juniper
Publishers please click on: https://juniperpublishers.com
For
more articles in Open Access
Journal of Dentistry & Oral Health please click on:


Comments
Post a Comment