Papillary Cyst Adenocarcinoma Arising in a Papillary Cyst Adenoma: A Rare Entity in the Sublingual Gland- Juniper Publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF DENTISTRY & ORAL HEALTH
Abstract
Papillary cyst adenocarcinoma (PCAC) of salivary
glands is an extremely rare, low-grade destructive tumor, with a
papillary - cystic architecture. PCAC has considerable overlap in
microscopic characteristics with the benign variant of papillary cyst
adenoma (PCA), where the main difference between the two is the presence
of frank invasion into surrounding tissues in PCAC. The present case
describes a long -standing lesion multilobulated submucosal mass of 4 cm
diameter of the floor of the mouth in a 78 years old female. Histologic
analysis reviled infiltrative pattern suggesting malignant pattern. The
history of a long duration with a recent increase in size, the
encapsulation of most of the tumor periphery and the localized front of
invasion, all suggest transformation from PCA to PCAC fiture of PCA.
Conclusion:n:With the results it is concluded that
preoperative plasma BNP levels is a reliable indicator for early
postoperative morbidity in patients undergoing coronary artery bypass.Keywords:Papillary cystic adenoid carcinoma
Introduction
Papillary cyst adenocarcinoma (PCAC) of salivary
glands is an extremely rare, usually low-grade destructive tumor, with a
papillary - cystic architecture, first classified as a distinct
neoplasm in 1991 by the World Health Organization (WHO) [1] and later by
Ellis and auclair [2]. It accounts for less than 0.2% of all salivary
gland tumors according to some studies [3,4,5]. Only a single lesion of
PCAC of the parotid was described within a series of 834 salivary glands
tumors [6]. The sublingual gland is an uncommon location for this
lesion [5]. PCAC has considerable overlap in microscopic characteristics
with the benign variant of papillary cyst adenoma (PCA), where the main
difference between the two is the presence of frank invasion into
surrounding tissues in PCAC.
In the following report we present a case diagnosed
as papillary cystadenoma of the sublingual gland in an incisional
biopsy, which following resection, turned out to have an area of
invasion and the final diagnosis was PCAC. The diagnostic challenges in
differentiating the benign from the malignant variants are discussed.
Case Report
A 78-year-old woman presented with an asymptomatic
mass of the floor of the mouth, left side. The patient was aware of
lesion in that area which was constant in size for a long duration, and
presented some growth 4 month prior to her examination. Clinical
examination revealed a multilobulated submucosal mass of 4 cm diameter.
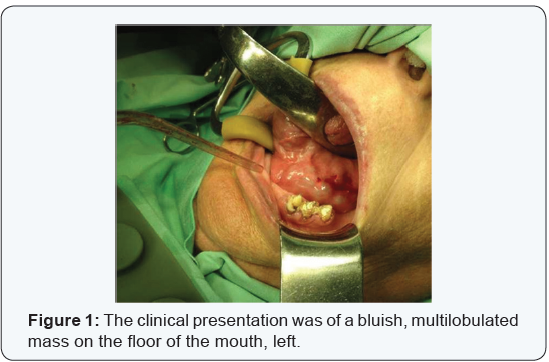
It was bluish, firm and the overlying mucosa was intact (Figure 1).
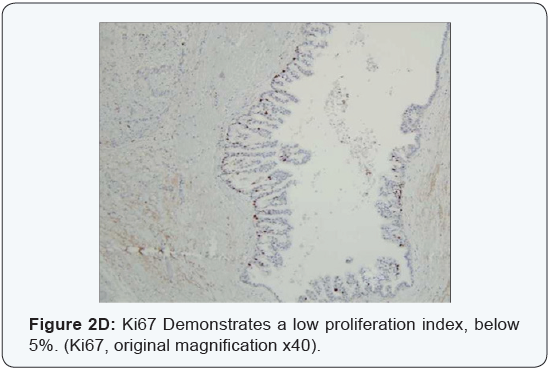
An incisional biopsy was performed, with the provisional
diagnoses including pleomorphic adenoma, adenoid cystic
carcinoma or mucoepidermoid carcinoma. Microscopic
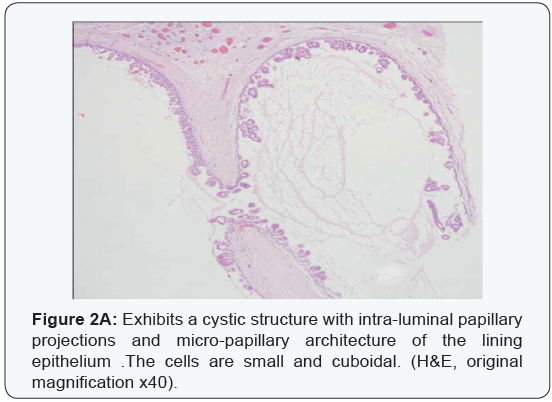
examination exhibited a multicystic architecture, lined by a
thin cuboidal epithelium, which proliferated to create small
and delicate intra-luminal papillary projections. The cells were
uniform, with a bland cytology, without atypia, prominent mitotic
activity or necrosis, and thus malignancy was not suspected at
this point. The biopsy was signed out as PCA (Figure 2a-2d).
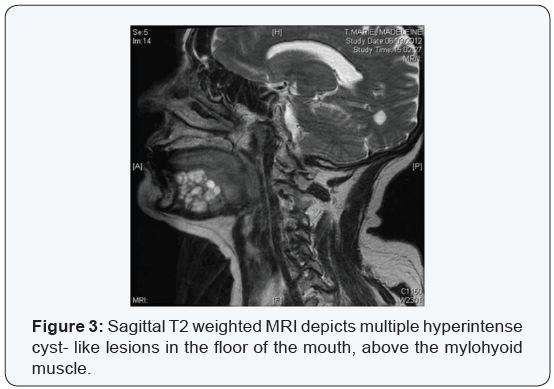
An MRI that was performed in order to define the extent and
nature of the lesion. A multicystic mass of 2cm X 3.2 cm X 4.5 cm
was identified in the left sublingual space above the mylohyoid
muscle. It was well circumscribed, did not involve the mandible
and lymph node enlargement was not observed. The left sublingual
gland could not be demonstrated in the MRI (Figure 3).
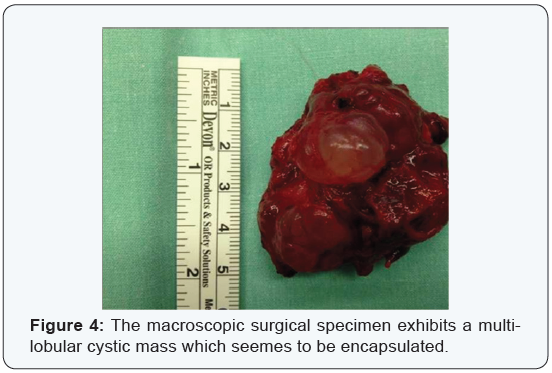
Under general anesthesia, a mucosal incision was preformed
above the mass. The lesion seemed to present a distinct
capsule, and an extra capsular dissection was carried out, with
the mass separating easily of from the surrounding tissues. In
the posterior aspect, a firm attachment to the submandibular salivary gland was observed, with no clear demarcation in that
area. The surgical specimen seemed macroscopically to be multilobulated,
well-circumscribed and encapsulated (Figure 4).
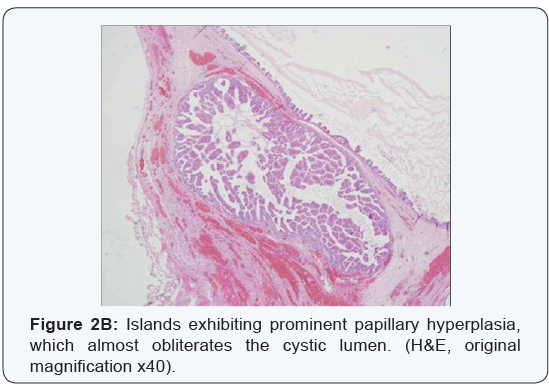
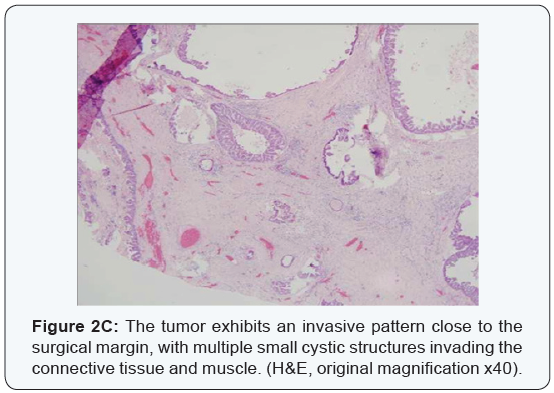
Multiple microscopic sections exhibited essentially the
same features described in the initial biopsy, with multiple
cystic structures, lined by thin bland cuboidal epithelium with
intra-luminal papillary projections. However, while examining
the margins it became evident that at least in one area (which
corresponded with the posterior aspect), the tumor had an
invasive pattern rather than a capsule, with multiple small
tumoral cysts and islands invading into the muscle. With this
finding the diagnosis was reversed from benign to malignant,
and signed-out as PCAC.
Discussion
Cystadenoma is characterized by epithelium-lined cystic
masses that contain secretion material, usually serous or
mucinous. When the tumor presents both papillary and cystic
features it is classified as PCA.
This tumor type is found in the ovaries, pancreas and salivary
glands. In the salivary glands it is most frequent in the parotid,
with decreasing incidence in submandibular, minor salivary
glands and the sublingual gland [7].
The World Health Organization (WHO) described PCA of
the salivary glands as a tumor that closely resembles Warthin
tumor but without the lymphoid elements, constituting multiple
papillary projections arising from undifferentiated epithelium of
the intercalated ducts of the glands [1,8].
In this variant the epithelial cells are typically tall and
present abundant eosinophilic cytoplasm, similar to Warthin’s
tumor. However, some cases present the same cystic papillary
architecture, but the cells tend to be small and cuboidal.
Salivary gland PCAC is an extremely rare malignant neoplasm,
with a peak of incidence in the 7th - 8th decades. A single case
of PCAC was described in a child [9]. The sublingual gland is an
uncommon location for this lesion. Foss et al. [6] described only
2 PCAC in the sublingual glands in a series of 57 PCAC cases.
Due to similar architecture and cytology, it may be difficult
to distinguish the benign variant (PCA) form PCAC, especially in
a biopsy specimen [10]. Both lesions lack overt atypia, necrosis
or prominent mitotic figures. In fact, the only definitive feature
separating PCA from PCAC is the presence of frank invasion in
PCAC, as opposed to complete encapsulation and absence of
invasion in PCA.
In the present case, the majority of the surgical specimen was
encapsulated clinically, with only one area in which the tumor
seemed to be inseparable from the surrounding tissues during
surgery. This area corresponded with the microscopic finding of
invasion into the peri-tumoral tissue. This fact, coupled with the
information the patient was aware of a mass which was constant
in size in that area for a long duration, and presented some growth
only 4 months prior to her examination, raises the possibility
of malignant transformation to PCAC in a long-standing benign
PCA. Similar processes are well recognized in other salivary
gland tumors, such as transformation to carcinoma- in- situ in
long standing pleomorphic adenoma, however, it has not been
described in these rare pair of PCA and PCAC [11].
Hence, once an incisional biopsy of PCA is signed out,
especially in long standing large lesions, the surgeon performing
the definite treatment and the pathologist should both keep
in mind there is a possibility of the lesion exhibiting invasive
features in the final surgical specimen, which would than require
re-classification from benign (PCA) to malignant (PCAC). Highgrade
variants may present cervical lymph node metastases
[6,12]. However, occasional cases of low grade PCAC with
cervical lymph nodes metastases have also been reported [13].
Local recurrences can occur at an average of 76 months after
initial treatment [6]. The treatment of PCA is surgical excision.
In most reported cases of PCAC an additional broader excision
or postoperative radiotherapy have been suggested and annual
revisions for a minimum period of five years [4,5,13,14].
For more Open Access Journals in Juniper Publishers please
click on: https://juniperpublishers.com
For more articles in Open Access Journal of
Dentistry & Oral Health please click on:

Comments
Post a Comment