Success and Survival Rates of Teeth Restored with Cast Post and Core among National Guard Health Affairs Patients, Riyadh, Saudi Arabia- Juniper Publishers
JUNIPER PUBLISHERS-OPEN
ACCESS JOURNAL OF DENTISTRY & ORAL HEALTH
Success and Survival Rates
of Teeth Restored with Cast Post and Core among National Guard Health Affairs
Patients, Riyadh, Saudi Arabia
Authored by Abeer A Al Subait
Abstract
Purpose:To determine the success
and survival rates of endodontically treated teeth restored with cast
post and core among NGHA patients in Riyadh, Saudi Arabia.
Materials and Methods:This
retrospective study was conducted in King Abdulaziz Dental Centre (KADC)
in Riyadh during November 2015 – April 2016. Fifty seven patients with
140 intraradicular cast posts were included. Patients were evaluated
both clinically and radiographically according to the FDI criteria for
the evaluation of direct and indirect restorations by two independent
examiners, one examiner for the radiographic and another for the
clinical examination, after obtaining a well-written and explained
informed consent form.
Results: Of 140 endodontically
treated teeth restored with cast post and core, 65 (46.4%) teeth showed
one or more of the radiographic failure and 76 (54.3%) showed one or
more clinical sign of failure. The accumulative failure rate was 72.9 %
which include relative failure of 45.0% and absolute failure of 27.9%.
The majority of the radiographic failure involve; periapical lesion
30.7% and recurrent caries 24.3%. The majority of the clinical failure
involve; dental caries 19.3% and periodontal pocket of more than 4mm
19.3%. The survival and success rate were 27.1% and 72.1% respectively.
Conclusion: Numerous
complications and high failure rate were noted among endodontically
treated teeth restored with cast post and core. This raise a question
about the validity of selecting cast post and core to restore
endodontically treated teeth in the presence of other advanced and
recent alternative intraradicular retention systems. However,
retrospective nature and small sample size caution us to conclude our
findings. Further randomized clinical trials are needed with long term
follow up period to build upon the findings of this study.
Keywords: Gingival recession; Core debonding; Post and core restorations; Incisors; PremolarsAbbreviations: ASA: American Academy of Anesthesiology; NGHA: National Guard Health Affairs; KADC: King Abdulaziz Dental Centre
Introduction
Endontically treated teeth usually require
intraradicular restoration for retention aspects due to extensive loss
of tooth structure resulting from caries, trauma and access cavity
preparation. Post and core restorations are usually used in root canal
treated teeth that require additional measures in order to receive
optimum restorations that adequately serve both functional and aesthetic
purposes. Post and core restorations with their different systems were
suggested as a successful method to increase retention for the coronal
restoration [1]. The most critical factor in avoiding complication with
intraradicular retention is preserving tooth structure [2,3]. In the
past, the most widely used post and core system was metal cast post and
core [4,5]. Furthermore, according to some, cast post and core
intraradicular retention system is still considered the established
technique or gold standard post system for restoring extensively damaged
and endodontically treated teeth [6,7]. This treatment modality has
maintained its popularity and credibility throughout the years.
Custom-fabricated post and cores using a standardized fabrication
technique have shown a good long-term prognosis with an average survival
time of 7.3 years [8]. Despite its popularity, cast post and core still
has many disadvantages such as root fracture, periapical lesion, and
dislodgment [9].
Furthermore, the introduction of other post systems
with comparable success and survival rates provides an alternative to
cast post system for root canal treated teeth [5]. Multiple in vivo
studies concluded low success rate and higher failure for cast post and
core such as in Ferrari et al in 1995, who found that cast
post and core showed high percentage of failure 14% and low
success rate 84% [9]. In 2007 found that failure rates of 8.82%
were observed in the cast metal post after 4 years of clinical
service [10]. Another study of GA Preethi et al. [11] found that the
success rate of the cast post and core was 90% after only one year
[11]. The range of survival rates of cast post and core - according
to Fokingga et al. [3] was between 78-94% [3]. Also in a number
of in vitro studies they found that the fracture resistance of cast
post and core is not the highest as has been advocated by clinical
expertise as demonstrated by Giovanni A et al. [12]. Abduljabbar
T et al. [13] found that the average load required to fracture cast
post & core systems was 541.2 N which is relatively comparable
to other systems.
Concerning fracture patterns, variety of studies showed that
most fracture patterns are usually unfavorable if they occur when
using cast post & core where fractures occurred in the tooth
structure [14]. In addition, Abduljabbar T et al. [13] concluded
that 90% of fracture patterns of teeth restored with cast post and
core were unfavorable (i.e. tooth is not restorable) [13]. In the
same topic a study was done by Salameh Z et al. [15] concluded
that teeth restored with cast post and core were significantly
more associated with unfavorable fracture with a percentage of
more than 50% of the study sample. Regarding the success rate in
relation to the type of tooth, GA Preethi et al. [11] in 2008 found
that cast post and core has the least success rate when used in
single rooted upper anterior teeth. While in an in vitro study done
by C.G. Castro et al. [16] studied if the type of tooth had any effect
in the fracture resistance, He found that canines and molars had
significantly higher values of fracture resistance than incisors and
premolars. The aim of this study is to determine the survival and
success rates of endodontically treated teeth restored with cast
post and core among patients of National Guard Health Affairs,
Riyadh, Saudi Arabia.
Methodology
This retrospective study was conducted in King Abdulaziz
Dental Centre (KADC) in Riyadh during November 2015 to April
2016. All medical record numbers for patients who received
cast post and cores were obtained from dental lab in KADC. Five
hundred and forty files were chosen using a simple random
sampling. Patients’ records were reviewed after obtaining the
permission from medical records department in KAMC. Based on
our inclusion and exclusion criteria sample size was 169 patients.
We excluded all those patient files which had
insufficient
information about the demographic data or contact information,
pregnant females and those who had other types of cement. Fifty
seven patients with 140 intraradicular cast posts were included
in this retrospective study. During the review of the included files,
information of age of the post, number of treated teeth, type of
cement, type of coronal restoration and whether the treatment
provider is a specialist or a resident were recorded using special form.
The selected patients were contacted by phone and invited
to participate in the study. The patients were provided with the
details of the evaluation. Subjects were invited to KADC clinics
for examination. Patients were evaluated both clinically and
radiographically according to the FDI criteria for the evaluation
of direct and indirect restorations by two independent examiners
after obtaining a well-written and explained consent form [17].
Every endodontically treated tooth with intraradicular cast
post and core system was evaluated both radiographically and
clinically. Radiographically by an intraoral periapical radiograph
taken by paralleling technique and interpreted for any recurrent
caries, periapical lesions, root fracture and furcation involvement.
Clinical examination done by using an explorer, periodontal
probe (William’s probe) and mouth mirror. Moreover patients
were investigated about any episodes of pain, pain on percussion,
discomfort or bleeding related to the tooth of interest and patients’
oral hygiene was evaluated by using Silness and Loe plaque Index
on Ramjford teeth. The assessment sheet included information on
patient’s age, gender, American Academy of Anesthesiology (ASA)
classification, tooth number and type and time the restoration
had been in clinical service. All outcomes were categorized as
relative or absolute failure. Any radiographic and clinical sign
of failure was considered as absolute failure. While presence
of either radiographic or clinical sign considered as a relative
failure. Success was defined as absence of absolute and relative
failure. Survival was defined as the absence of absolute failure
[18,19]. Patients with failed post and cores were referred to the
dental clinics for further management. The data were analyzed
using SPSS software. A P value of 0.05 and less was considered
statistically significant.
Results
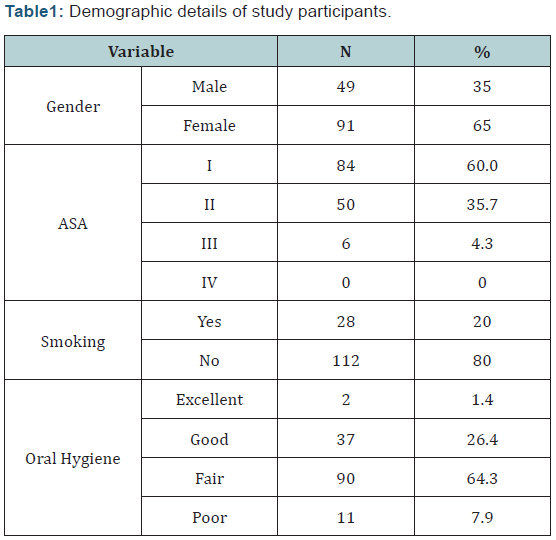
In this study 140 teeth, of whom 91 (65%) belonged to female
patients and 49 (35%) to male patients, were examined at the
dental center of King Abdulaziz Medical City (Table 1). The age of
the patients ranged between 17 to 82 years old with a mean age
of 40 years. Eighty four (60%) patients claimed they do not have
any medical condition, while 56 (40%) claimed to have at least
one medical condition. Of the total teeth the majority of the teeth
were molars and premolars – 103 (73.6%) – while 37 (26.4%)
were incisors and canines The posterior teeth have higher failure
rate comparing to the anterior teeth with the difference being
statistically not significant (P=0. 071).Treatment was provided by
either a specialist 92 (65.7%) or resident 48 (34.3%). The failure
rate was higher among teeth which had been treated by resident
however the difference being statically insignificant (P=0.348).
Regarding smoking, 10 (17.6%) of the patients were smokers
while 47 (82.4%) were nonsmokers. The failure in smokers was
not statistically significant (P=0.193) when compared to nonsmoker
patients. One of the major factors for having healthy
dentition was good oral hygiene practice. The patients in this
study had different oral hygiene status ranging from excellent 2 (3.5%), good 20 (35.1%), fair 28 (49.1 %) and poor 7(12.3%).
The result showed that the difference in oral hygiene status had
no significant effect in relation to the failure (P =0.999). The
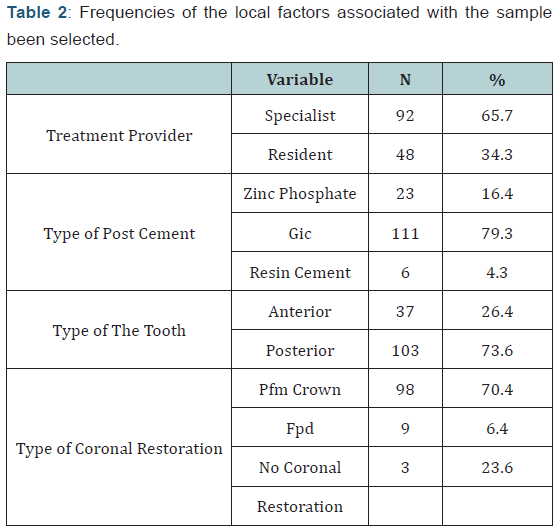
post were cemented using GIC, resin cement and zinc phosphate
cement with a percentage of 79.3%, 4.3%,and 16.4% respectively.
The difference among the different types of post cement in
relation to the failure was not statistically significant (P=0.42).
Ninety eight (70%) of the total teeth were restored with Porcelain
Fused to Metal for single crowns while 9 (6.4%) were used as
abutments for fixed partial denture. The other 33 (23.6%) teeth
were left without a final restoration (Table 2). The final restoration
showed insignificant difference (P =0.058) in relation to failure.
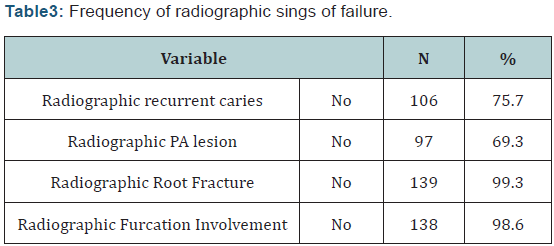
The radiographic failure includes presence of one or more of the
following: recurrent caries, periapical lesion, root fracture, and
furcation involvement (Table 3). Sixty five (46.4%) of the teeth
showed at least one of the radiographic failure signs. Thirty
four (24.3%) of teeth have radiographic recurrent caries while
43(30.7%) have radiographic periapical lesion. Radiographic root
facture and furcation involvement was in 1(0.7%) and 2(1.4%)
teeth respectively Seventy six (54.3%) of the teeth showed one or
more signs of the clinical failure which include: spontaneous pain,
tenderness to percussion, caries, periodontal pocket of more than
4 mm, gingival recession, post and core debonding, post and core
fracture, furcation involvement, mobility of post (Table 4). Only
3(2.1%) of the teeth had spontaneous pain while 4(2.9%) teeth
were tender to percussion while 27(19.3%) teeth showed signs
of recurrent caries clinically. Regarding periodontal problems,
27(19.3%) teeth have periodontal pocket more than 4mm while
17(12.1%) teeth have gingival recession. Nine (6.4%) of the post
were debonded where 16(11.4%) of the post were mobile. Neither
post and core fracture nor furcation Involvement was seen. The
total failure rate which includes both absolute and relative failure
was in 72.9 % of the teeth.
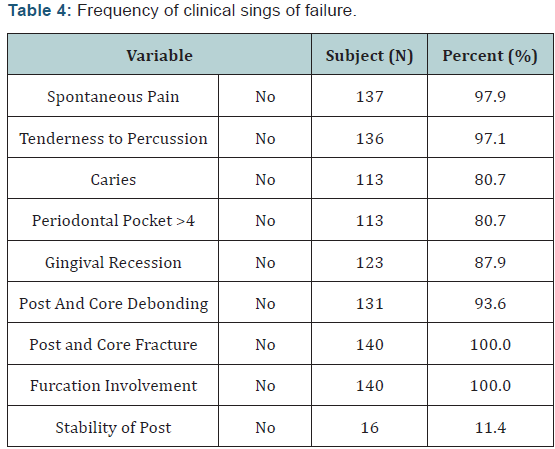
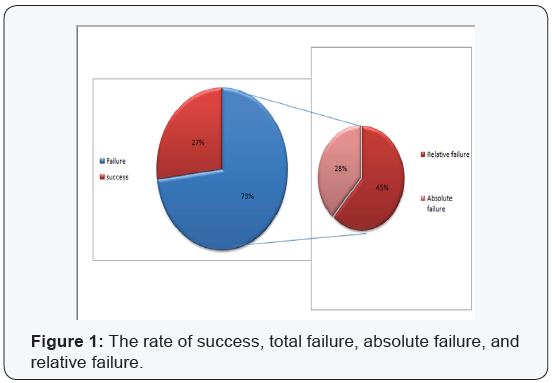
The absolute failure includes both clinical and radiographic failure and the rate was 27.9%. While the relative failure involves all teeth that have either clinical or radiographic failure the rate was 45.0%. On the other hand, teeth which did not show any sign of clinical and radiographic failure were consider succeeded. The success rate of the total sample size was 27.1% (Figure 1) while the survival rate was 72.1%.
Discussion
This retrospective study was conducted on 140 teeth belongs
to both male and female subjects and aimed to determine
the survival and success rates of endodontically treated teeth
restored with cast post and core .The success rate was around
one third of the total sample while the survival rate exceeded
two thirds. Regarding the absolute and relative failure rates, they
were observed among one third and half of the study sample
respectfully. Failure rates due to caries and periodontal pockets
were the highest among the teeth having clinical failure while
periapical lesions were the most prevalent cause of radiographic
failure.
The strength of the present study include: the level to which
inclusion and exclusion criteria were set to meet, the informed
consent which was obtained from all subjects, both male and
female participants were included with multiple diversities
and variations, examination was done both clinically and
radiographically according to FDI criteria, patients that required
further treatment and management were referred to be treated
per complaint and at the end, outcomes of the study were clearly
defined and all predictors for failure were analyzed. Regarding
the sample distribution, the majority of our sample belongs to a
middle age group who are classified as ASAI due to the fact that
our study is both clinically and radiographically based which
requires the presence of the patient in dental office that may
be a challenge to elderly and/or patients with serious medical
problems. Furthermore, most of the samples were posterior teeth
restored with PFM crowns which are because posterior teeth
have relatively less esthetic demands and require load-bearing
restorations [20].
The high survival rate shown in our study goes along with
what was proven by other studies as in Balkenhol et al. [21] which
concluded that the survival probability of cast post and cores
reaches up to 7.3 years. Also, Heydecke et al. [1] in his literature
review mentioned that survival of cast post and cores ranges
from 87.2 to 88.1%. The failure rates which were observed more
in female patients who constituted the bulk of the study sample
contradicts what was mentioned in Hikasa et al. [22] where he stated that failure rates of cast metal posts and cores are more
associated with males rather than females. In the same study
it was mentioned that the higher the age of the patient at the
cementation of the cast post and core the higher the failure rates
observed which is in accordance with our findings.
The relative high survival rate showed in this study in the
posterior teeth restored with cast post and core has been noted
by Mentink et al. [7] who reported high survival rated among
posterior teeth. The relative high failure rates observed among
teeth treated by residents can be due to the wrong case selection
and treatment planning errors as shown in Sarkis et al. [23] who
concluded that dentists without post-graduate training used cast
post and core more frequently as their first choice.
Although it was not statistically significant, smoking was more
associated with higher failure rates, this can be explained by Tomar
et al. [24] and Jang Ay et al. [25] where they found that smoking
constitutes a risk factor for periodontal disease which may affect
the longevity and survival of affected teeth. All teeth-related and
patient-related factors addressed in this study such as type of
tooth, final restoration, type of cement used, oral hygiene status
and the ASA classification of the patients showed no influence on
the success and survival rates. This can be explained in one way or
another by the small sample size of the study which was the result
of our restricted inclusion criteria requiring meticulous details in
the documentation of each case.
When comparing the failure rates between the different
cements included in this study, GIC had the most failure rates
which contemplates what was mentioned in Zheng et al. [26]
where he concluded that using GIC cement significantly aggravates
coronal microleakage. The low success rate can be attributed to
the fact that teeth requiring intracranial retention are usually
severely destructed with little or no coronal structures which
further compromises their long term prognosis as shown in
Ferrari et al. [19]. In fact, most of our sample had fair to poor oral
hygiene and reported that there were no follow up appointments
which indicates that there weren’t any kind of maintenance that is
recommended in complex treatments involving multidisciplinary
interventions.
All teeth-related and patient-related factors addressed in
this study such as type of tooth, final restoration, type of cement
used, oral hygiene status and the ASA classification of the patients
showed no influence on the success and survival rates. This can
be explained in one way or another by the small sample size of
the study which was the result of our restricted inclusion criteria
requiring meticulous details in the documentation of each case.
The resultant success and survival rates were influenced by the fact
that different treatment phases were done by different providers
from the endodontic treatment through prosthodontic procedures
and restorations. However, the sample included only teeth treated
according to standards protocol which were illustrated in the
patient file. Nevertheless retrospective nature of study caution
us to conclude our findings as there are many factors that could have resulted in endodontic failure. As survival rates depend
upon tooth structure, cause of RCT, operator technique, sourced
of contamination, type and quality of post and coronal restoration.
Many of these factors are not studied in this present study.
Moreover the method in which this study was conducted
limits us in matters of sampling and insurance of optimum dental
management throughout the different phases subsequent to and
after cementation of the cast post and cores. So, a randomized
clinical trial raising the same question with better sampling
techniques and more involvement in all treatment steps would
carry out highly reliable results and interpretations which can be
of benefits in understanding the value of this treatment modality
in relation to all alternatives and how it can be provided in high
quality manner.
Conclusion
Numerous complications and high failure rate were noted
among endodontically treated teeth restored with cast post and
core. This raise a question about the validity of selecting cast post
and core to restore endodontically treated teeth in the presence
of other advanced and recent alternative intraradicular retention
system. However, retrospective nature and small sample size
caution us to conclude our findings. Many other factors are needed
to be explore as failure rates are highly dependent on many vital
factors related to the tooth structure, reason for RCT, time span,
type of techniques used by clinician and many other factors that
can confound study results. Nevertheless Further randomized
clinical trials are needed with long term follow up period to build
upon the findings of this study.
For more Open Access Journals in Juniper Publishers please
click on: https://juniperpublishers.com
For more articles in Open Access Journal of
Dentistry & Oral Health please click on:

Comments
Post a Comment