Peripheral Odontogenic Fibroma: A Case Report and Review of The Literature- Juniper Publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF DENTISTRY & ORAL HEALTH
Peripheral Odontogenic Fibroma: A Case Report and Review of The Literature
Authored by Zuyan Zhang
Abstract
Peripheral odontogenic fibroma (POF) is a rare
odontogenic tumor, characterized by a fibrous or fibromyxomatous
proliferation that contains varying amounts of odontogenic or presumed
odontogenic epithelium, occasionally with the presence of dentin or
cementum like bodies or other forms of calcification. Peripheral
odontogenic fibroma is often misdiagnosed as fibrous epulis and easily
confused with peripheral osteofibroma. Pathological examination is the
only diagnostic approach for peripheral odontogenic fibroma, which can
provide a basis for treatment and prognosis evaluation. Radical surgical
resection is the most common treatment for this disease. This report
presents a clinical case of a 35-year-old female patient boy with a
gingival overgrowth along the left first mandibular molar, which was
diagnosed as peripheral odontogenic fibroma.
Keywords: Peripheral Odontogenic Fibroma; Gingiva; Inflammatory Hyperplasia
Abbreviations: ODF: Odontogenic
Fibroma; POF: Peripheral Odontogenic Fibroma; COF: Central Odontogenic
Fibroma; POT: Peripheral Odontogenic Tumor
Introduction
Odontogenic fibroma (ODF) is described as “a rare
odontogenic tumor, benign neoplasm of odontogenic ectomesenchymal
origin” classified by the World Health Organization, characterized by
relatively mature collagenous fibrous tissue with varying amount of
odontogenic epithelium [1]. Odontogenic fibroma can occur in central or
peripheral location. The peripheral odontogenic fibroma (POF) is
considered to be the mucosal counterpart to the central odontogenic
fibroma (COF) [2]. Odontogenic fibroma comprises only 0.05% in all
odontogenic tumors [3]. Peripheral odontogenic tumor (POT) is rare,
while peripheral odontogenic fibroma may be the only peripheral
odontogenic tumor with occurrence rate more than corresponding
intraosseous lesions, it being more common compared to central
odontogenic fibroma by a 1.4:1 ratio [4].
Peripheral odontogenic fibroma presents a
slow-growing, progressive but painless swelling, often associated with
cortical expansion or tooth displacement [5]. There is a slight female
predominance in literatures [6]. This disease frequently occurs in the
30-40 years of age [6]. There is no significant difference in the
distribution of the upper and lower jaw. The attachment gingivas of
molars or premolars are most predilection sites [7].
Peripheral odontogenic fibroma is characterized by a
fibrous or fibromyxomatous proliferation that contains varying amounts
of odontogenic or presumed odontogenic epithelium, occasionally with the
presence of dentin or cementum like bodies or other forms of
calcification [8]. Pathological examination is the only diagnostic
approach for peripheral odontogenic tumor, which can provide a basis for
treatment and prognosis evaluation.
The purpose of this article is to report the clinical
and histopathological features of a case of peripheral odontogenic
fibroma in a 35-year-old female patient.
Case Report
A female patient aged 35 years, reported to the
department of periodontology with a chief complaint of progressive
swelling along the lower left back tooth for 5 months. She had slight
discomfort in this area. This tooth accepted root canal therapy 1 year
ago. And the patient was in good general health. The intraoral
examination revealed gingival neoplasia in the buccal gingiva of the
left first mandibular molar, with a size of 7*7*5 cm3, with a hard
texture, red color, and a clear boundary (Figure 1). The patient had a
little tenderness on palpation. The temporary sealing material presented
on the occlusal and distal surfaces of the tooth, which was partially
detached with lingual
gingival in growth. There was a little food impaction between the
left first and second mandibular molars. The probing depth of the left
first mandibular molar was 3~4mm and the tooth had
no mobility. There were no obvious images of alveolar bone
resorption and apical lesions on periapical film.

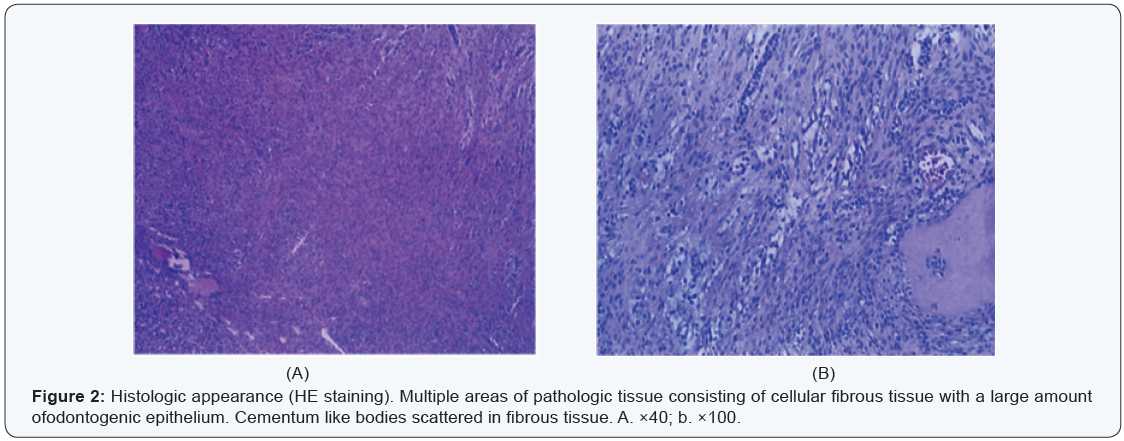
The surgery was conducted under local anesthesia. The tumor and tissues 1-2 mm around the lesion was completed excised. The lingual gingival enlargement was also removed. On histopathological examination, the Hematoxylin and eosin stained soft tissue section confirmed the diagnosis of peripheral odontogenic fibroma accompanied by inflammation. Besides, there were induced phenomena in some regions (Figure 2).
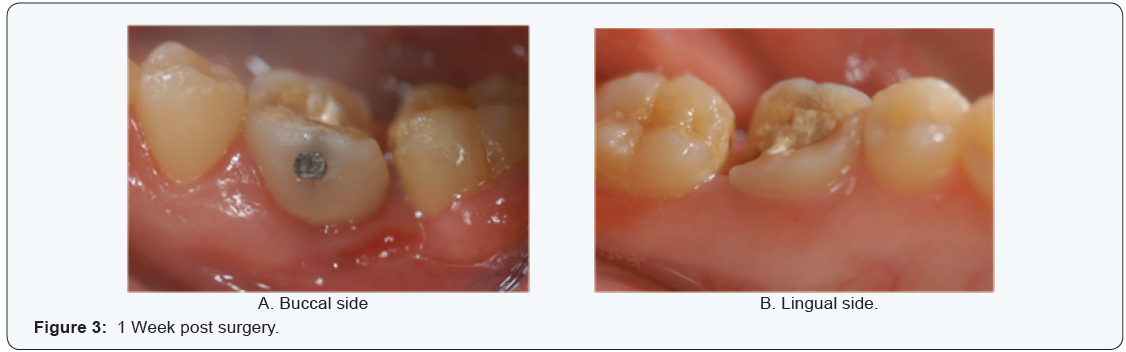
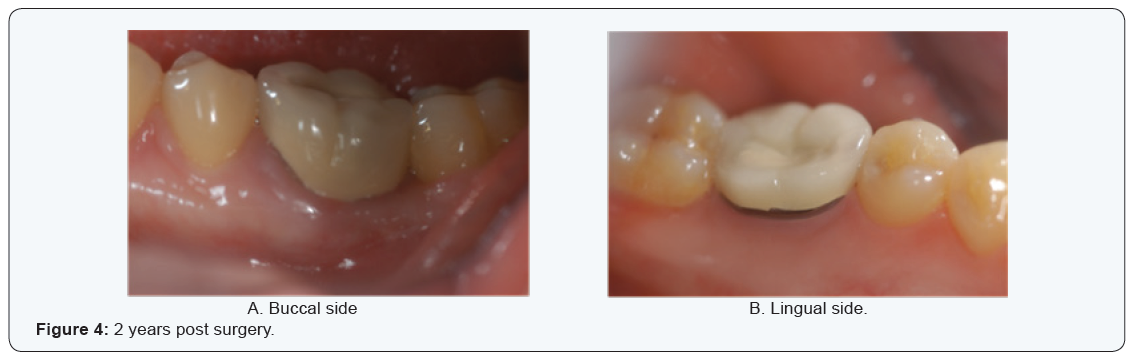
The patient was instructed to rinse with 0.12% chlorhexidine twice a day for a week. The patient was followed up with at 1 week (Figure 3), 1 month, 3, 6, 12, 18 and 24 months after surgery. At 1month after surgery, the left first mandibular molar was restored with a porcelain crown. No recurrence was observed at 2 years post surgery (Figure 4).
Discussion
Peripheral odontogenic fibroma is the rare peripheral
counterpart of central odontogenic fibroma. It is an apparently
innocuous, elevated gingival lesion that has no conclusive
data regarding its exact prognosis. It is generally believed that
peripheral odontogenic fibroma originates from mesenchymal
tissue [9]. Radical surgical resection is the most common
treatment for this disease [10]. A recurrence rate of 13% after
resection has been reported in the literature [11]. It has been
stated that budding of the basal cell layer of the surface squamous
epithelium is associated with a higher recurrence [12]. Although
the epithelium appears to have diagnostic significance in the
lesions, it is stable and non-neoplastic [13].
Peripheral odontogenic fibroma is often misdiagnosed as
fibrous epulis and easily confused with peripheral osteofibroma.
The latter is a reactive lesion, derived from the periosteum and
can produce osteoid and woven bone [14]. Histological features
of peripheral odontogenic fibroma is cellular fibrous tissue
or fibrous and mucous tissue proliferation, containing varying
amounts of odontogenic epithelium, and occasionally dentin,
cementum like bodies, bone tissue or other forms of calcification
[8].
Peripheral odontogenic fibroma occupies nearly 40%
of peripheral odontogenic tumors [15]. Most of peripheral
odontogenic tumors have similar clinical manifestations and
differential diagnosis, which are similar to benign reactive
lesions. However, there are little local stimulating factors for
them, and they have a certain recurrence rate after local excision
[16,17]. Therefore, it is suggested that peripheral odontogenic
tumors should be long-term followed up.
Acknowledgement
The authors are grateful to Dr. Bingbing Li (department of
Pathology & Laboratory Medicine, Peking University, School and
Hospital of Stomatology), for her great help and support.
For more Open Access Journals in Juniper Publishers please
click on: https://juniperpublishers.com
For more articles in Open Access Journal of
Dentistry & Oral Health please click on:

Comments
Post a Comment