Infected Periapical Cemental Dysplasia of the Mandible a Surgical Approach: Case Report- Juniper Publishers
JUNIPER PUBLISHERS-OPEN
ACCESS JOURNAL OF DENTISTRY & ORAL HEALTH
Infected Periapical Cemental Dysplasia of the Mandible a Surgical
Approach: Case Report
Authored by Federico Lamus
Abstract
Osseous dysplasias are non-neoplastic benign
fibrous-osseous lesions that result from a localized change of normal
bone in which all the components of cancellous bone are replaced by
fibrous and cementum like tissues containing different amounts of
abnormal appearing bone. The solitary (monostotic) type which occurs
typically in middle age; the mean age is 39 years and occurs nine times
more often in females than males and almost three times more often in
blacks than in whites, it’s also frequently seen in Asians. Cone Beam
Computed Tomography (CBCT) has become a commonly used diagnostic tool in
Dentistry when periapical surgery is contemplated to be able to gain
knowledge about the relationship of the lesions and their neighboring
anatomical features.
Case Presentation
A 66 year old Asian Female presented to our office
for her 3 month routine periodontal maintenance appointment, her health
history was evaluated and the patient had been diagnosed with high blood
pressure and epilepsy, conditions for which she was taking Depakote and
Mavik, no history of Biophosphonate intake, heavy bleeding and
suppuration was reported by the hygienist during probing at the location
of tooth #19 (distal) (Figure 1).
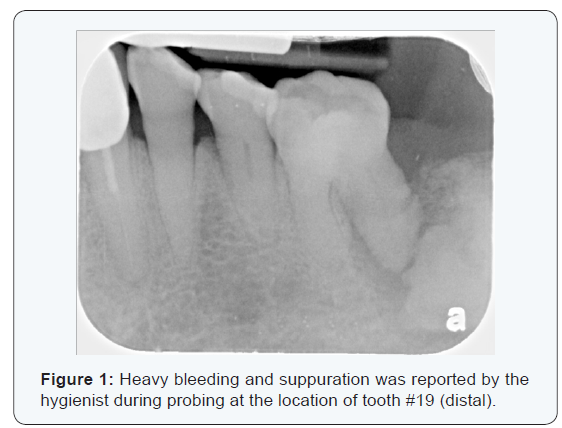
A fibrous osseous lesion, diagnosed as Periapical Cemental Dysplasia had been noted on the chart as an incidental finding during the evaluation of a small full mouth survey taken 5 years earlier, everything had been found to be within normal limits and free of symptoms at the time of the initial examination, the Periodontist examined the patient after the hygienist informed her of the finding, upon clinical inspection it was found that tooth #19 had mobility class lll, deep pocketing (12 mm), profuse bleeding, suppuration and pain upon percussion and pressure tests, the tooth was deemed non-restorable due to the advance state of deterioration in the periodontal tissues and an extraction of the tooth was recommended, she was referred to the Oral Surgeon. The tooth (#19) was removed by the Oral surgeon under local anesthetic using 72 mg of Lidocaine 2% using an inferior alveolar block and the tooth was removed without complications.
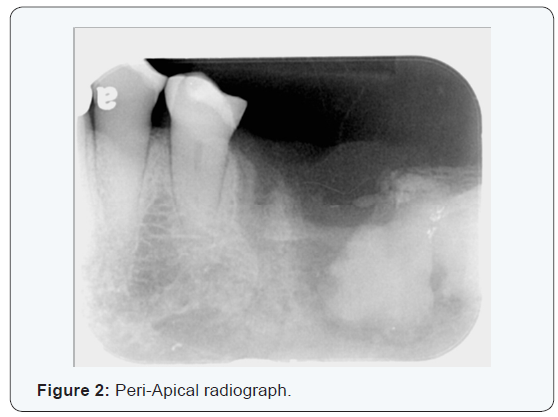
Two months later the patient presented to our office with a chief complaint of purulent drainage coming from the extraction site of where tooth #19 was located at along with mild vestibular swelling and erythema, a Peri-Apical radiograph was taken and revealed increased lucency around the previously noted fibrous osseous lesion, no history of pain, trismus and airway issues were noted. She was placed on 500 mg of Cipro orally every 12 hours for one week and was scheduled for a re-evaluation with the Oral Surgeon one week later. A week later the patient presented with purulent discharge still present but no pain or bleeding was noted at the time (Figure 2). A CBCT scan was taken to evaluate the lesion, size, location and vital structures associated with the it; A limited Volume maxillofacial non-contrast, thin slices (0.133μm resolution), Cone-Beam CT, 85 kV 10mA for 6s, (503mGy.cm²) of the left body of the mandible was taken.
General Findings
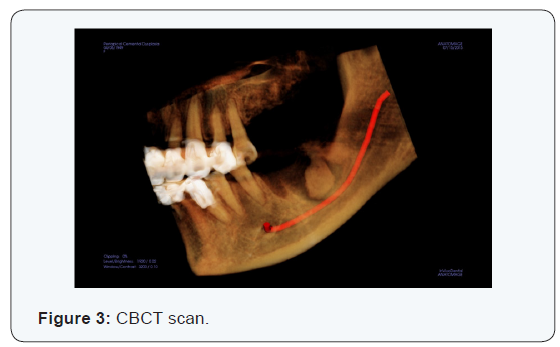
Teeth # 8, 9,14-19, 23 & 24 are not present on the volume
obtained, there are coronal restoration on teeth # 10, 11, 12 & 22 (Figure 3)
Specific Findings
On the left body of the mandible there is radiopaque entity
(Figure 4,5) surrounded by a radiolucent band at the level of where
teeth # 17-19 were located at, the radiolucent band encapsulates
the entire lesion and the width is approximately 2mm in
its entirety, the radiopaque lesion measures approximately
10.65mm (mesial-distal) x 7.62mm (buccal-lingual) x 14.35
mm (coronal-apically), the lesion has similar density as dental
root structure, the lingual cortical plate is slightly expanded, the
lesion reaches the inferior alveolar canal and the coronal-buccal
aspect of the lesion appears to be thinning the cortical plate with
evidence of dis-rupture noted.
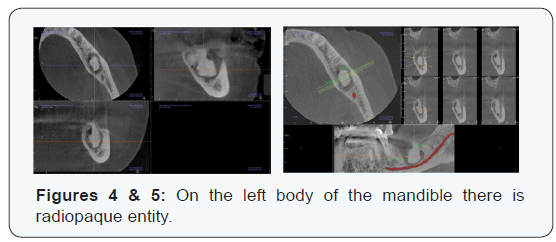
There is no clinical report of any paresthesia. The radiographic impression was periapical osseous dysplasia with an infected involucrum [1]. The treatment plan presented was for surgical removal and biopsy of the infected involucrum under local anesthesia [2].
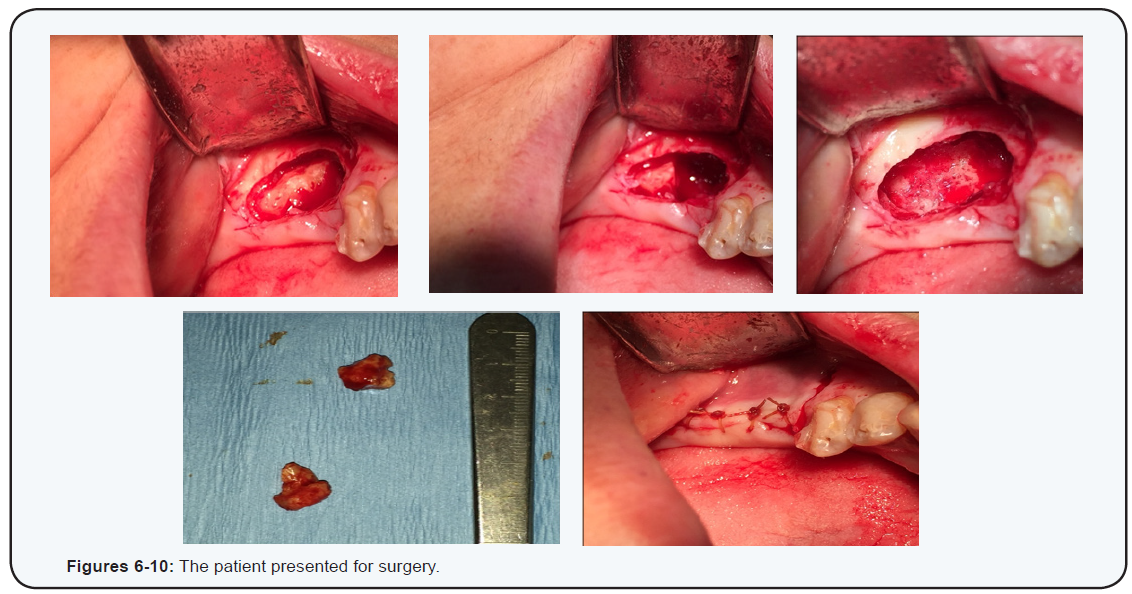
The patient presented for surgery (Figures 6-10) and the involucrum was removed under local anesthetic using 108 mg of lidocaine 2% with epinephrine 1:100.000, the lesion was approached form the most coronal aspect, sectioned in two and removed with a gross description of two fragments of tan-brow hard tissue measuring 2x1x1.5 cm placed in aggregate), the patient was sent home and a Medrol Dose Pack (methylprednisolone) was prescribe [3-5].
The specimen was submitted for decalcification with
a clinical impression of Periapical Osseous Dysplasia, the
diagnosis was returned as a Non-Vital Hard Tissue with Abscess,
with microscopic description of dense fragments of non-vital
cemento -osseous hard tissue with necrotic marrow spaces and
associated abscess and some areas of fibro-vascular marrow consistent with an infected benign fibro-osseous lesion (Osseous
dysplasia) [6].
Two weeks later the patient presented for removal of sutures
and post operative check up, she reported no pain, numbness,
bleeding or suppuration. Six months later the patient presented
for follow up Cone Beam CT (Figure 11,12), a CBCT scan was taken
for post operative evaluation, a limited Volume maxillofacial noncontrast,
thin slices (0.133μm resolution), Cone-Beam CT, 85 kV
10mA for 6s, (503mGy.cm²) of the left body of the mandible was
taken. The scan revealed the entire area where the lesion was
located at was filled with a fibrous healing defect (see arrows on
the selected reformatted images). The patient has been followed
in our practice has been symptoms free for 6 months and is ready
for rehabilitation via removable partial dentures.
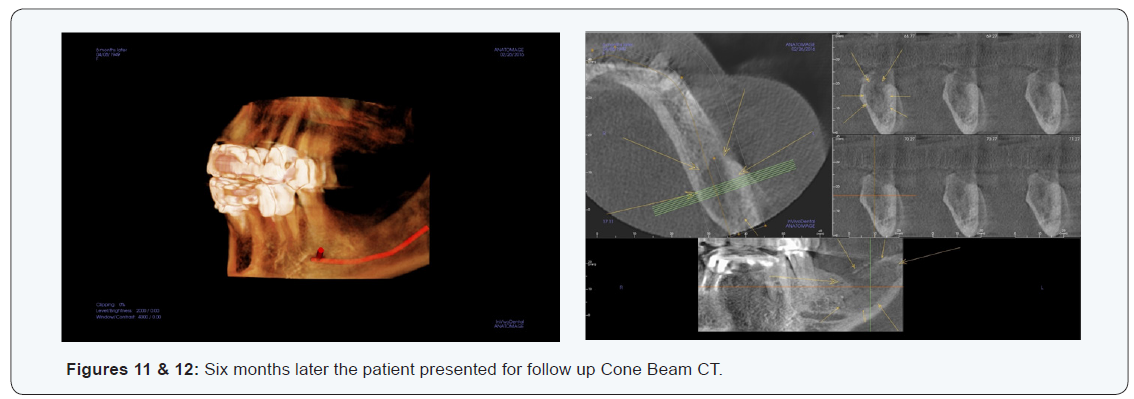
Note: Multiplanar reformatting was carried out at the work station using InVivo5 Software, with selected images which were adjusted for viewing and are not actual size scale, any measurements or recorded markers have been made in the primary image fields and are included only as guidelines not as substitute for complete analysis using the primary imaging series. Measurements provided are estimates, and may not represent the exact dimensions; actual dimensions will depend on slice selection and orientation. The use of intra-oral radiographs for assessment of caries and periodontal disease was recommended.
For more Open Access Journals in Juniper Publishers please
click on: https://juniperpublishers.com
For more articles in Open Access Journal of
Dentistry & Oral Health please click on:

Comments
Post a Comment