Emulating Natural Morphology in Anterior Crown Fractures: Two Years Follow-up Report-Juniper Publishers
Juniper Publishers - JuniperPublishers-DentistryOralHealth
Authored by Parisa Foroughiasl
Abstract
Patients may suffer from undesirable aesthetic
problems due to color, shape and structural or position abnormalities of
anterior teeth. Crown fractures are one the most common reasons of
these aesthetic complaints especially in young patients. Creating a
conservative as well as powerful restoration against destructive
occlusal forces while emulating similar outlook to natural dental
tissues is the main objective of treatment of such cases. Direct
composite resin restorations are one of the best possible treatment
options for the anterior crown fractures. As the dental materials and
techniques develop, the clinicians start to learn the physical and
optical properties of these materials and use them with proper
techniques to create more natural alike as well as long lasting
restorations. These restorations are no longer named as 'day savior
fillings' today but are called minimally invasive, functional and long
lasting 'direct aesthetic restorations' that perfectly emulate natural
dental tissues even in anterior area. This article illustrates how to
perform a minimally invasive, long lasting, functional and natural alike
direct aesthetic restorations in a single visit.
Keywords: Crown fracture; Direct aesthetic restorations; Emulating natural tissues
Objective
Performing a minimally invasive, long lasting,
functional and natural alike direct composite resin restorations in a
single visit.
Introduction
Aesthetic restoration of lost dental tissues of
anterior teeth is a crucial challenge in restorative dentistry. Patients
may suffer from undesirable esthetic problems due to color, shape,
structural and position abnormalities of anterior teeth. Creating more
conservative as well as more powerful restorations against occlusal,
lateral and protrusive forces and emulating similar outlook to natural
dental tissues is the main objective of up-to- date, contemporary
dentistry [1].
An increasing number of dentists prefer minimal invasive and less
time-consuming treatment options; as direct resin restorations compared
to indirect ceramic restorations for the anterior dental aesthetics [2].
In order to create more natural-looking restorations, clinicians must
learn and understand the physical properties of the dental tissues and
restorative materials that they use and also interactions of these
tissues and materials with light [3].
Various dental materials and techniques have been coming on the scene
to improve both functional and aesthetic quality of the restorations.
However a few of the esthetic resin materials on the market meet the
expectant. The ones having such properties such as simplicity,
structural stability, surface polish ability, masking discolorations,
surface texturing and simulating natural dental color parameters such as
hue, value and chrome are one step ahead [4,5].
Clinical considerations
In this report complex crown fractures due to dental
trauma on maxillary right central and lateral incisors were corrected
with minimally invasive direct composite resin restorations by using
layering technique in a single appointment. The composite resin material
used in this case study is a recently developed resin based restorative
material, Estelite Asteria (Tokuyama, Japan) designed for emulating
natural dental tissues.
Case Report

17 years old female patient applied to the clinic with aesthetic complaints due to dental trauma. He had direct trauma to the maxillary incisors a year ago and had no pain or any other symptoms. According to the intraoral examination complex crown fractures on maxillary right central and lateral incisors were determined (Figure 1,2).
According to the radiographic and vital metric
analysis the injured teeth were considered as vital. The periodontal
tissues were healthy and oral hygiene was in good condition. The
patient' s age and the examinations were both taken into consideration
and a conservative approach, minimal invasive direct aesthetic resin
restorations were considered as the treatment plan.
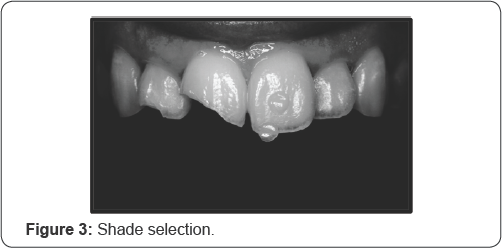
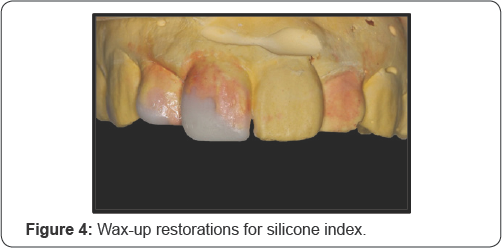
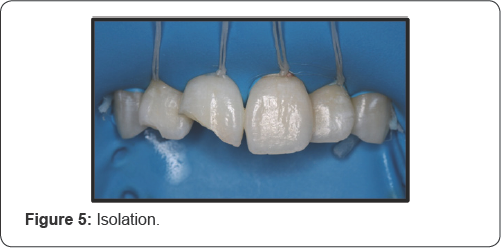
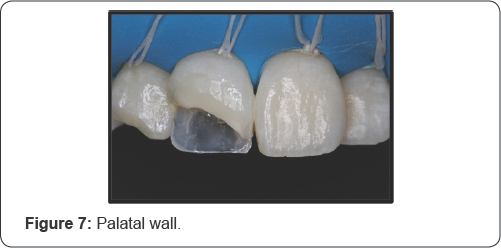
Shades selected by using macro dental photography and composite shade samples which are also known as the 'Button Technique. Most appropriate body and translucent shade samples of Estelite Asteria (Tokuyama, Japan) were selected and located on the crown of left central incisor. The body shades were located on the mid-third and the translucent shades were located on the incisal-third of the crown. Then a macro photograph was taken from the labial view by using a professional camera set designed especially for dental photography. The set consist of a body (D700), a macro lens (Macro 100mml), a macro twin flash (MT- 24EX Macro Twin Late Flash), two-sided reflectors and a dual flash bracket mount (Novo Flex Unset). The picture taken was processed in a computer software program called Adobe Photoshop CC (Photoshop CC, Adobe Systems Software). A processed black and white form of the photograph was used to decide the translucent shade. Another processed copy on which contrast was increased and brightness was decreased, was used to decide the body shade (Figure 3). A1B and NE shades (Estelite Asteria, Tokuyama, Japan) were selected. Temporary restorations were prepared for the cracked teeth on a cast model and silicone impression was taken to create a palatal silicone index (Figure 4). Rubber dam was applied on maxillary incisors and canines for maximum isolation (Figure 5). 45 degree deep beveling were done on both incisors to cover the crack lines as minimally invasive preparations (Figure 6. One bottle universal adhesive agent (Bond Force II, Tokuyama, Japan) was used with selective etching. The translucent shade composite resin, NE shade, was used to create the palatal enamel wall. The resin was placed on incisallt on the silicone index and refined by using a composite brushed wetting resin. Then the resin and the silicone index were placed intraoral on the palatal surface of the teeth and polymerized. The index removed and palatal enamel wall was created (Figure 7).

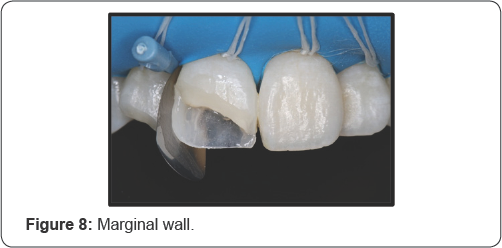
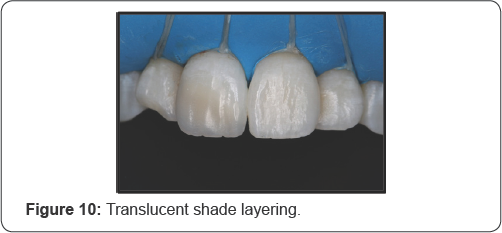
The same resin was used to create marginal enamel walls of the restorations by using kidney-shaped metal matrix bandstand wedges (Figure 8). Body shade composite resin, A1B shade, was used to emulate dentin tissue (Figure 9). Labial surface was restored by using the translucent shade resin (NE) to create the surface enamel layer (Figure 10). In order to avoid overcontouring, composite brush was used with the wetting resin for layering. The surface structure was also created in final surface layering step. The resin used for emulating the enamel surface layer was applied in 3 steps; medial third, distal third and middle third, so that creating the surface grooves, ridges and also incisal notches while layering. The irregular scratches on the surface were emulated by using the composite brush gently without wetting resin (Figure 11).

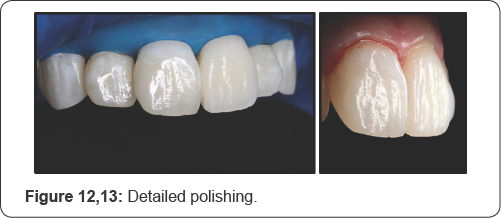
After polymerization of the last layer, glycerin (Air
Barrier, GC, Japan) was applied to whole the restoration surfaces and
polymerized for 40 seconds to eliminate the oxygen inhibition layer. The
surface cleaned with water spray and dried with air spray. Marginal
adaptations and removal of excessive resins were done by a #12 lancet, a
fine-grained composite polishing disk (Soflex, 3M, Japan) and interface
sandpapers (Epitex, GC, Japan). The labial surface was polished by
using only a fine-grained spiral rubber disc (Twist-Dia, light blue) in
low speed and in dry condition (Figure 12,13).
The patient was informed about the oral hygiene and informed for recalls for every 6 months (Figure 14).

At 2years recall no sensitivities, fractures,
secondary caries lesions were detected on both the teeth and the
restorations. Also no discolorations or demarcation lines were detected (Figure 15,16).

On the other hand the micro surface morphology on the
central incisor, created with brush touches while layering, was barely
may observed. The patient reported that the restorations were fully
functional during the time and he was also very satisfied with the
aesthetic result. Oral hygiene and periodontal health were also in good
condition (Figure 17).
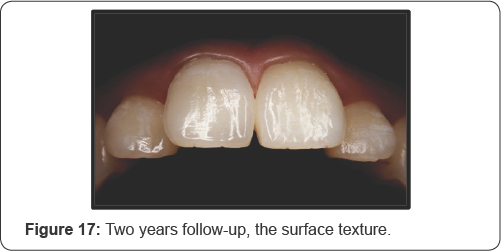
Considering all, in 2 years follow-up the structural
integrity, the color stability as well as the aesthetic outlook of the
restorations was considered as satisfactory. The patient was called for
further follow-ups.
Discussion
Ever increasing aesthetic demands of the patients
require better dental materials and application techniques and also more
clinical experience and knowledge. Natural-looking as well as
functional and stable dental restorations may only be created only with
the combination of these headlines. Natural dental tissues demonstrate
translucency, opalescence, and fluorescence that must be imitated by the
chosen restorative material in order to emulate the natural [6,7].
Especially translucency is recently accepted to have a key role in
shade match of the restorative materials with natural dental tissues.
Translucency is defined as the amount of light that passes through the
dental tissues and may vary according to one of the parameters of color,
value [8]. If the value of a tooth or dental material is high, lighter reflect from the surface, resulting in low translucency [9].
Taken this into consideration, some dental manufacturers have developed
some new generation of aesthetic composite resins to emulate the
natural dental tissues better than ever.
In the case presented a recently produced Estelite
Asteria (Tokuyama, Japan) was used as the composite resin material which
has supra-nano inorganic spherical fillers. Although this resin has an
advantage for using as two-step layering, in this case conventional
three-step layering was used to mimic the natural dental tissue layers.
The composite brush manipulation was very easy and effective while
layering as the consistency of the resin was soft enough. It is a fact
that the composite layering procedures under reflector light takes much
longer time that might be a problem. But the working time of the shades
of this resin was also long enough. The polymerizing time for the shades
used in this study was 10 seconds that is an advantage for the
clinician. The natural surface morphology was emulated with gentle brush
touches while surface layering. As the method used for layering depends
on not creating over-contouring, the polishing procedures for
restoration surfaces only done by a fine grained spiral polishing disc
(Twist Dia, light blue). The surface texture created by composite brush
hits could only be protected by using this polishing procedure [10].
This polishing material also creates a very shiny surface that is also
very resistant to discolorations. Smooth adaptation between resin and
dental tissues and having no micro-leakage due to the enhanced physical
properties of the resin such as low polymerization shrinkage may
describe having no sensitivities or secondary caries at 2 years recall [11].
As the correct indication of the case is an indispensable condition for
direct anterior resin restorations, the stability of the restorations
depends on having no devastating occlusal forces. The restorations were
fully functional during the 2 years time and had no fractures as a
result of that [12].
The enhanced fracture resistance of the composite resin might also
positively affect the strength of the restorations. Also the glycerin
(Air Barrier, GC, Japan) used for enhancing the physical properties of
the surface layer made a positive effect on creating a more resistant
surface layer to potential fractures and discolorations [13].
The loss in micro surface morphology on the central incisor that was
created with brush touches may be related to the erosive or abrasive
pattern of patient's diet and brushing style. It may be due to the
surface roughness of the restoration which is related to the physical
properties of the resin used. However that loss was insignificant for
the aesthetic outlook in speaking distance. The patient was very
satisfied with the durability, aesthetic outlook and especially the
color harmony and gloss of the restorations. The specific spherical
fillers and enhanced optical properties of the resin [14], the button technique used for selection of the shades [15], overcontour less layering technique [8,16] and detailed polishing procedures [17] are possibly played the key roles in this aesthetic outcome.
For years the anterior direct resin restorations
compared to the indirect veneers and accepted as a loser in general.
They were blamed as weak especially about durability and color
resistance. However before criticizing, everyone must self-criticize
him/ herself and ask the question: if these direct restorations were
done correctly or not? Like all dental procedures, direct composite
resin restorations have some indications and contra-indications. These
can be aliened as; proper occlusal relations [18], correct shade selection [19], good isolation [20], good adhesion [21], detailed polishing [22], frequent recalls [18,21] quality materials [18]
and also clinical experience. These are like rings of a circle and if
one of them breaks, then the whole restoration fails. If the direct
composite resin restorations were performed by taking these into
consideration, the success rate of these restorations would definitely
increase.
Conclusion
As a conclusion although 2 years times still a short
term to evaluate, with correct indication, quality material and proper
technique the direct resin restorations were seemed to be highly long
lasting, color resistant and aesthetic under the conditions of this
follow-up case study If direct restorations with composite resins are
done by the rules, they are obviously one of the best treatment options
for today's dentistry.
For more Open Access
Journals in Juniper
Publishers please click on: https://juniperpublishers.com
For more articles
in Open Access Journal of Dentistry & Oral Health please click
on: https://juniperpublishers.com/adoh/classification.php
To know more about Peer Review Journal of
Dentistry & Oral Health

Comments
Post a Comment