Oral Health, Diseases, Examination, Diagnosis, Treatment Plan &Mouth Preparation- Juniper Publishers
Juniper Publishers - Open Access Journal of
Dentistry & Oral Health
Oral Health, Diseases, Examination, Diagnosis, Treatment Plan &Mouth Preparation- Juniper Publishers
Abstract
Aim of the study: To research the perceptions of patients in the Diyarbakir region in respect of the toxicity of mercury in amalgam fillings.
Materials and methods:The study
included 500 patients with at least one amalgam filling who attended the
clinic for routine dental treatments. Data were gathered using a
single-page questionnaire The questions on the form related to age,
gender, marital status, level of education, economic status, types of
dental filling, whether or not the amalgam filling included mercury and
whether or not mercury was harmful to human health. Questions were also
asked to ascertain the patient’s level of knowledge in respect of
mercury, amalgam fillings and human health.
Results:A total of 500 patients were
included in the study, comprising 283 (56.6%) females and 217 (43.4%)
males. When economic status was questioned, 267 (53.4%) patients
reported monthly income of 0-1000TL and 233 (46.6%) patients reported
more than 1000TL. The level of education was primary school in 110 (22%)
patients, high school in 159 (31.8%), university or post-graduate in
190 (38%) and 41 (8.2%) were illiterate. The type of dental filling was
unknown by 64.4% of patients and 59.6% did not know that the amalgam
filling contained mercury. 52.6% of the patients did not know whether or
not mercury was harmful and 72% did not know whether or not mercury in
amalgam was harmful.
Conclusion:A low level of awareness was determined in the study participants in respect of the toxicity of mercury in amalgam fillings.
Keywords: Awareness; toxicity; Mercury; Dental AmalgamIntroduction
The oral cavity composed of:
a. Hard tissues as: Bones of the upper jaw (maxilla ) & lower jaw ( mandible ), bone of the palate, and teeth.
b. Soft tissues as: Periodontium, soft palate, tongue, floor of the mouth, cheeks & lips.
The most common diseases always affect the teeth and the periodontium.
The Periodontium is composed of :
Gingiva:The normal gingiva is firm and pink in color and composed of :
a) Free gingival:It is the movable
part of the gingiva that extent from the gingival crest to the bottom of
the gingival sulcus (normal sulcus depth is 1-2 mm).
b) Attached gingival:It is the stippled part of the gingiva.
Periodontal ligaments:The
periodontal ligaments are arranged in 5 bundles in different directions.
It is responsible for the nutrition and attachment of the teeth in
addition to act as foundation for the prosthesis.
Alveolar bone crest:The alveolar
bone crest is 2 mm away from the gingival sulcus. The periodontium is a
connective tissue structure attached to the periosteum of both the
maxilla & the mandible that serves to anchor the teeth in the
maxillary and the
mandibular alveolar processes. It provides attachment & support,
nutrition, synthesis & resorption, and mechanoreception.
The main element of the periodontium is the periodontal
ligament (PDL), which consists of collagenous fibers (Sharpey’s
fibers), embedded in bone and cementum, and giving support to
the tooth in function.
There are five principal fiber groups in the PDL that traverse
the space between the tooth root & alveolar bone, providing
attachment and support :-
- Trans-septal fibers: extending interproximally between adjacent teeth; their ends embedded in cementum.
- Alveolar crest fibers: beginning just apical to the epithelial attachment and extending from cementum to the alveolar crest.
- Horizontal fibers: coursing at right angles from cementum to the alveolar bone.
- Oblique fibers: extending in an oblique direction apically, attaching cementum to the alveolar bone. They are the most numerous fibers.
- Apical fibers:radiating from cementum into the alveolar bone at the apex of the root.
There are also smaller irregularly arranged fibers
interspersed between the principal fiber groups. Cellular
elements found in PDL included - fibroblast [the main synthetic
cell, producing collagen & other proteoglycans], cementoblasts
& cementoclasts, osteoblasts & osteoclasts, and mast cells &
epithelial rests [playing a role in pathologic conditions of the
periodontium].
At the base of the gingival sulcus is the epithelium - tooth
interface named dentogingival junction (DGJ). This structural
relationship between hard and soft tissues is unique in the
body, which anchor the epithelial cells to the enamel and
cemental surfaces. The depth of the sulcus is variable in healthy
individuals, averaging 1.8 mm. In general, the shallower it is, the
more likely is the gingiva to be in a state of health.
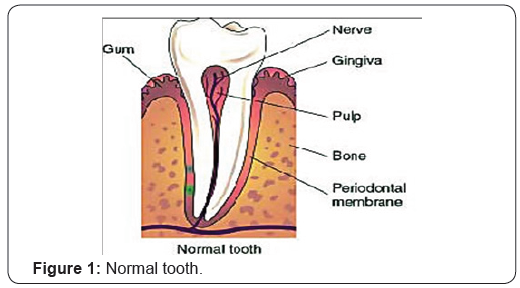
The Tooth is composed of :
- Enamel:The hardest outer part of the tooth composed from enamel prisms embedded in a matrix which bonds the prisms together.
- Dentin:The resilient part of the tooth which contains tiny tubes called dentinal tubules through which pass nerve filaments to collect at the junction between enamel & dentin ( dentino- enamel junction ) forming the nerve plexus.
- Pulp:The soft connective tissues contain blood vessels and nerves, and fill the inner space of the tooth which called pulp chamber & root canal. It is responsible for nutrition of the tooth & sensation.
- Cementum:The outer layer of the root covering the dentin. It is responsible for attaching the 5 bundles of PDL from one end to insure tooth anchor (Figure 1).
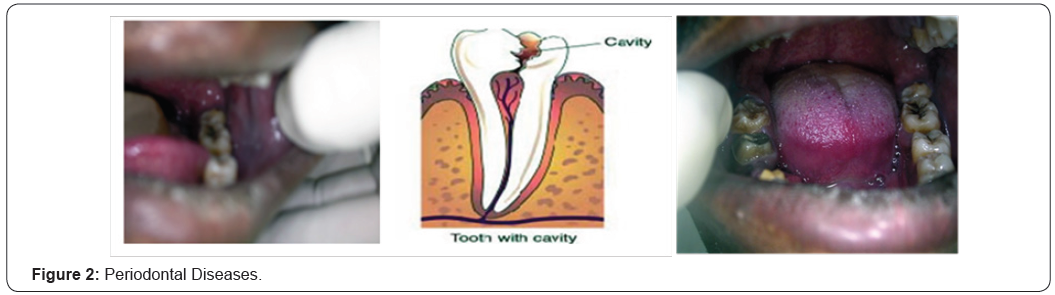
Common Oral Diseases
Tooth decay
Tooth decay, which is also called dental cavities or dental
caries, is the destruction of the outer surface (enamel) of a tooth.
Decay results from the action of bacteria that live in plaque, which
is a sticky, whitish film formed by a protein in saliva (mucin) and
sugary substances in the mouth. The plaque bacteria sticking
to tooth enamel use the sugar and starch from food particles
in the mouth to produce acid. Tooth decay is a common health
problem, second in prevalence only to the common cold. It has
been estimated that 90% of people have at least one cavity,
and that 75% of people had their first cavity by the age of five.
Although anyone can have a problem with tooth decay, children
and seniors are the two groups at highest risk. Other high-risk
groups include people who eat a lot of starchy and sugary foods;
people living in areas without a fluoridated water supply; and
people who already have numerous dental restorations (fillings
and crowns).
Etiology and prognosis
Tooth decay requires the simultaneous presence of three
factors: plaque bacteria, sugar, and a vulnerable tooth surface.
Although several microorganisms found in the mouth can
cause tooth decay, the primary disease agent appears to be
Streptococcus mutans. The sugars used by the bacteria are
simple sugars such as glucose, sucrose, and lactose. They are
converted primarily into lactic acid. When this acid builds up
on an unprotected tooth surface, it dissolves the minerals in the
enamel, creating holes and weak spots (cavities). As the decay
spreads inward into the middle layer (the dentin), the tooth
becomes more sensitive to temperature and touch. When the
decay reaches the center of the tooth (the pulp), the resulting
inflammation (pulpitis) produces a toothache. The general term
periodontal disease is used to describe any condition of the
periodontium other than normal (Figure 2).
Etiology
Most gingival & periodontal diseases result from microbial plaque. Other contributors to inflammation, however, are calculus, acquired pellicle, materia alba, and food debris.Terminology
Microbial plaque:It is a sticky substance composed of
bacteria & their byproducts in an extra cellular matrix & also
containing substances from the saliva, diet, and serum. It is
basically a product of the growth of bacterial colonies & is the
initiating factor in gingival & periodontal disease.
Calculus:It is a chalky or dark deposit attached to the tooth
structure. It is essentially microbial plaque that has undergone
mineralization with the passage of time.
Acquired pellicle:Pellicle is a thin brown or gray film of
salivary proteins that develops on teeth after they have been
cleaned. It frequently forms the interface between the tooth
surface and dental deposits.
Materia alba:It is a white coating composed of
microorganisms, dead epithelial cells, and leukocytes that is
loosely adherent to the tooth. It can be removed from the tooth
surface by water spray or by rinsing.
Pathogenesis:Sequence of events in the development of
a gingivitis - periodontitis lesion is a very complex. It involves
not only local phenomena in the gingiva, PDL, tooth surface,
and alveolar bone, but also a number of complex host response
mechanisms.
The chronic plaque induced lesion has been investigated &
analyzed, so, divided into initial, early, established, and advanced
stages.Tooth Loss:
- Trauma: Trauma due to accident may cause:
- Avulsion of tooth from its socket.
- Fracture of the tooth crown with part of the root.
- Internal fracture of the root with separation of the fractured part.
- Alveolar bone fracture with gingival trauma and exposure of the root to oral cavity.
- Unrestorability: Unrestorability of the tooth may be due to:
- Mutilation from caries with complete destruction of the crown and part of the root.
- Root caries with fraction involvement.
- Failure to do R.C.T for the tooth.
- Occlusion & path of insertion problems: Severe tilting of the tooth which causing problem with occlusion & fabrication of other prosthesis.
- Periodontal problems: Severe periodontal problems which cause looseness of the tooth or furcation involvement with other complications as caries of roots & furcation area (Figure 3).
Introduction
Fixed Prosthodontics treatment can offer exceptional
satisfaction for both patient & dentist. It can transform an
unhealthy, unattractive dentition with poor function into a
comfortable, healthy occlusion capable of giving years of further
service, while greatly enhancing esthetics. To achieve that goal,
meticulous attention to case selection through right diagnosis,
treatment planning & mouth preparation must be done within
the first visit in sequence, with great accuracy.
Diagnosis
Diagnosis is defined as “The procedures of collecting data
and information through different channels, so that, a proper
line of treatment can be proposed. “
Fundamentals of diagnosis are- History
- Examination
- Articulated Diagnostic Casts
History
Chief Complaint:Is the patient’s primary reason (s) for
seeking treatment.
It’ll be one or more of 4 categories- Comfort: discomfort may be from pain, sensitivity or swelling.
- Function: malfunction may be during mastication or speech.
- Social: unpleasant appearance may be due to mouth bad taste or odor.
- Appearance: unpleasant appearance may be due to bad restoration or teeth discoloration (Figure 4).

Personal Details:Name, age, sex, address, education,
occupation, marital status, children, and telephone number
Medical History:Could be achieved under 4 categories :
- Conditions affecting the treatment methodology, e.g., any disorders that necessitate the use of antibiotic premedication, any use of steroids or anticoagulants, & previous allergic response to medication or dental materials.
- Conditions affecting the treatment plan, e.g., previous radiation therapy, hemorrhagic disorders, extremity of age, and terminal illness.
- Systemic conditions with oral manifestations, e.g., + Periodontitis= diabetes, menopause, pregnancy, or the use of anticonvulsant drugs. + Erosion of teeth= stomach acid regurgitation in case of hiatal hernia, bulimia, or anorexia nervosa. + T.M.J. disorders or reduced salivary flow= as side effect of certain drugs.
- Possible risk factors to dentist & auxiliary personnel, e.g., patients who are suspected or confirmed carriers of hepatitis, AIDs, or syphilis.
Dental History: Includes :
- Periodontal history and oral hygiene
- Restorative history: filling and F.P.Ds
- Endodontic history
- Orthodontic history
- Removable Prosthodontic history
- Oral surgery history
- Radiographic history
- T.M.J. dysfunction history
Methods of Clinical Examination
General examination
General appearance, skin color, and vital signs as respiration,
pulse, temperature, and blood pressure.
Extra oral examination: special attention to facial
asymmetry = may hint at serious conditions.
Cervical lymph nodes are palpated, as are the T.M.J., & the
muscles of mastication. Lips position during smiling is critical in
treatment planning.
Intra oral examination: Reveals considerable information
concerning the condition of the soft tissues, teeth, and supporting
structures. Lips tongue, floor of the mouth, vestibules, cheeks,
and the hard & soft palates are examined; and any abnormalities
are noted.
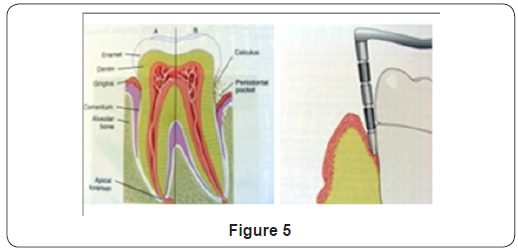
A.Periodontal examination:
- Gingiva: Color, texture, size, contour, consistency, and position.
- Periodontium: Pocket’s depth, tooth mobility or malpositions, open or deficient contacts, and furcation involvement must be recorded after thorough examination (Figure 5).
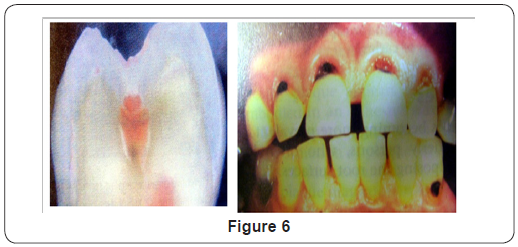
B. Diagnosis of caries:Accurately diagnosing early
dental caries is a challenge for the dentist. The following
methods are used for detecting dental caries, and each has
specific limitations:-
- Dental explorer: When a sharp explorer tip is pressed into an area of suspected caries, it will “stick” when being removed. N.B. This technique is not effective in diagnosing carious lesions on teeth that have been exposed to fluoride.
- Radiographs: Although useful for detection of interproximal caries, early caries on occlusal surfaces is not visible on radiographs. In addition, the extent of caries can easily be misdiagnosed because the caries is often two times deeper and more widespread than it appear on the radiograph.
- Visual appearance: The appearance of dark-stained grooves in the teeth may indicate caries. However, the grooves may simply be stained from coffee or tea (Figure 6).
- Laser caries detector: The recently introduced laser caries detector is used to diagnose caries and reveal activity under the enamel surface. A small battery-operated unit directs a laser beam into the tooth. When the beam encounters a change in the integrity of the tooth, it gives off a fluorescent light of different wave-lengths. The laser caries detector is equally effective in both primary & permanent teeth. The laser wave-length is translated through the handpiece into a number from 0 - 99, according to the degree of fluorescence based on the amount of decay. The laser cannot be used to diagnose inter-proximal caries due to the limited access. In addition, it cannot detect caries under dental sealants or amalgam restorations (Figure 7).
C. Diagnosis of teeth required R.C.T:The diagnosis
of a tooth requiring endodontic treatment is based on an examination that has both subjective and objective
components.
Subjective examination:includes an evaluation of
symptoms or problems described by the patient, which include
the following:
- + Chief complaint
- + Character and duration of pain
- + Painful stimuli
- + Sensitivity to biting and pressure
- + Extent of caries
- + Periodontal conditions surrounding the tooth in question
- + Presence of an extensive restoration
- + Tooth mobility
- + Swelling or discoloration
- + Pulp exposure (visual examination)
Several techniques are used to test pulp vitality in
determining whether endodontic treatment is required or the
pulp is still vital and able to repair itself.
When testing a questionable tooth, a control tooth is selected
for comparison ( healthy tooth, usually of the same type, in the
opposite quadrant ). The use of control tooth shows that the
stimulus is capable of achieving a response.
Methods of vitality evaluation
- a. Percussion & Palpation:Are tests used to determine whether the inflammatory process has extended into the periapical tissues. Positive test results indicate that there is inflammation in the periodontal ligament and the endodontic treatment is required.
- b. + Percussion test:by tapping on the occlusal or incisal surface of the tooth with the end of the mouth mirror handle, which is held parallel to the long axis of the tooth?
- c. + Palpation test:by applying firm pressure to the mucosa above the apex of the root.
- d. - Thermal sensitivity:Are tests with temperature extremes to determine the status of the pulp. The thermal stimulus is never placed on a metallic restoration or the gingival tissue, which would result in an abnormal response and could cause damage to the tissues.
- e. + Cold test:The dentist uses ice, dry ice, or ethylchloride to determine the response of a tooth to cold. The control tooth and the suspect tooth are isolated and dried, then the source of cold is applied first to the cervical area of the control tooth, and after to the cervical area of the suspect tooth.
- f. + Heat test:Is generally the least useful of the vitality tests because a painful response to the heat could indicate either reversible or irreversible pulpitis. Only, the necrotic pulp will not respond to the heat. A small piece of guttapercha, or the end of an instrument, is heated in a flame and applied to the facial surface of the tooth.
- g. - Electric pulp testing:is used to determine whether a pulp is vital or non-vital. Like other testing devices, it can produce a false response; therefore, the test results must be supported by other diagnostic findings.
Electric pulp testers deliver a small electrical stimulus to the pulp. Factors that influence the reliability of the pulp tester include the following:
- Teeth with extensive restorations can vary in response.
- In teeth with more than one canal, one canal may be vital and the others may be non-vital.
- A failing pulp can produce a variety of responses.
- Control teeth may not respond as anticipated.
- Moisture on the tooth during testing may produce an inaccurate reading.
- 6- The batteries in the tester may weaken over time.
- - Cavity test: By the use of small inverted cone carbide bur with high speed hand-piece, a small cavity done without using anesthetic solution. If the suspect tooth is vital the patient will feel pain. This test is only used, if there is still doubt about the tooth vitality.
- - Radiographic evaluation: radiographs are a necessity for diagnostic testing as well as in root canal treatment. Good quality radiographs are required for optimal information.
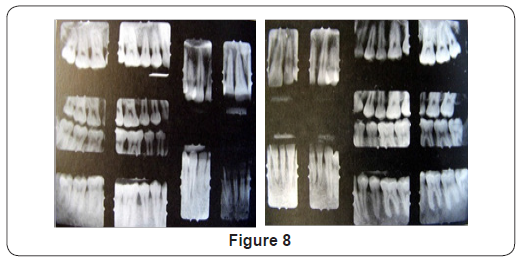
D.Radiographic full-mouth examination:
1. Intra-oral full-mouth radiographs:are composed
of both periapical and bite-wing films. They are used to examine the teeth and the supporting structures. For the
average adult, a full-mouth series consists of 18 - 20 films are
needed. Occlusal films, also, are needed to detect the position
of impacted teeth, or a lesion in bone (Figure 8).
2. Extra-oral & digital radiography:provides an overall
image of the skull and jaws. In some cases the extra-oral film
is used because the patient has swelling or severe pain and
is unable to tolerate the placement of intra-oral films. It may
be used alone or in conjunction with intra-oral films. The
images seen on an extra-oral film are not as well defined or
as sharp as the images seen on an intra-oral radiograph.
Indications for extra-oral radiographs are:- - To identify trauma or fractures.
- - To determine the size and area of large lesions.
- - To identify T.M.J. disorders.
- - To detect diseases of the jaws.
- - To identify the location of impacted teeth.
- - To determine jaw growth and development.
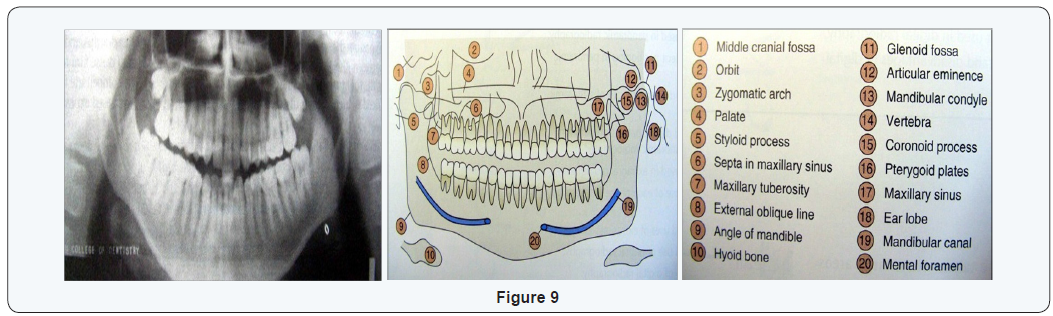
3. Panoramic radiograph:allow the dentist to view the
entire dentition and related structure on a single film.
Intra-oral films are used to supplement a panoramic film for
detection of dental caries or periapical lesions (Figure 9).
4. Lateral jaw radiography:is used to view the posterior
region of the mandible. It is very useful in children, patient with
limited jaw opening, and patients who cannot tolerate intra-oral
film placement.
5. Skull radiography:is used most often in oral surgery
and orthodontics.
The most common skull radiographs used in dentistry
include the following:
+ Lateral cephalometric:is used to evaluate facial growth
and development, trauma, and disease & developmental
abnormalities.
It shows the bones of face and skull as well as the soft tissue
profile.
+ Posteroanterior:is used to evaluate facial growth
& development, trauma, and disease & developmental
abnormalities.
It shows the frontal & ethmoid sinuses, the orbits, and the
nasal cavities (Figure 10).

+ Waters projection:is used to evaluate the sinus area. It
shows the frontal and ethmoid sinuses, the orbits, and the nasal
cavities.
+ Submentovertex: is used to identify the position of the
condyles, show the base of the skull, and evaluate fractures of the
zygomatic arch. Also, shows the sphenoid and ethmoid sinuses
and the lateral wall of the maxillary sinus.
+ Reverse towne:is used to identify fractures of the
condylar neck and ramus. Imaging technique:- as the T.M.J. area
can be very difficult to be examined radio-graphically because of
the multiple adjacent bony structures, also radiography cannot
be used to examine the articular disc and other soft tissues of the
T.M.J.. Instead, special imaging techniques such as arthrography
& MRI must be used.
6. Digital radiography:uses an electronic sensor to
record the penetration of the x-ray photons and then sends
this information to a computer that digitizes these electronic
impulses. This allows the computer to produce a diagnostic
image on a monitor almost instantaneously.
E. Occlusal examination :
- General alignment.
- Lateral and protrusive contacts.
- Centric relation.
- Jaw maneuverability (Figure 11).

A. Articulated diagnostic casts:They are essential in
treatment planning. Static and dynamic relationships of the
teeth can be examined without interference from protective
neuro-muscular reflexes. The unencumbered views reveal
aspects of the occlusion not detectable within the confines of
the mouth.
+ Steps for accurate diagnostic casts are :-
- B. Impression making:Accurate alginate impression of both dental arches are required.
- C. Articulator selection:Articulators are classified according to how they can reproduce mandibular border movements.
Types of articulators are:
- 1. Small non adjustable articulators:Don’t have the capacity to reproduce the full range of mandibular movement. Their use often leads to occlusal discrepancies.
- 2. Semi adjustable articulators:Are the practical approach to provide the maximum diagnostic information. Two types: arcon & non arcon. The mechanical fossa, in an arcon type, is fixed relative to maxillary cast, where as in the non arcon design it is fixed relative to mandibular cast; thus the arcon is anatomically correct.
- 3. Fully adjustable articulators:Are instruments with wide range of positions that can be set to follow patient’s border movements.
- 4. Face bows:Used to record the spatial position of the maxillary arch relative to the opening and closing axis. They are rigid caliper-like devices that permit some adjustments to be made.
- Kinematic hinge axis face bow.
- Arbitrary hinge axis face bow.
2 types:
D. Centric relation record:Provides the orientation of
mandibular to maxillary teeth at CR in the terminal hinge position,
where opening & closing are a purely rotational movement. Casts
articulated in the IP don’t permit evaluation of the CR & contact
relationships. Therefore, the relation of diagnostic casts in CR is
of significant diagnostic value.
E. Jaw manipulation:Accurately mounted casts depend
on precise manipulation of the patient’s mandible by the dentist.
The condyles should remain in the same place throughout the
opening - closing arc. The load - bearing surfaces of the condylar
processes, which face anteriorly, should be manipulated into
apposition with the mandibular fossae of the temporal bones,
with the disc properly interposed. The best technique to be used,
is “Dawson” technique.
Anterior programming device, plastic leaf gauge, or
cotton rolls, can be used first to prevent tooth contact before
manipulation to ensure that there are no muscular reflexes
during manipulation (Figure 12,13).


+ Uses of articulated diagnostic casts are:-
I) Distribution & dimensions of edentulous span:
- 1. Distribution of edentulous are:could be properly evaluated to decide whether to construct R.P.Ds or F.P.Ds.
- 2. Mesio - distal dimension:Short M.-D. width = short span Long M.-D. width = long span, leads to bending of the bridge, therefore increase the number of the abutments and F.-F. type is indicated.
- 3. Occluso - gingival height:this will determine the type of the selected pontic & retainers.
II) Type of bite & occlusal prematurities:The main
advantage of the study cast is to study the “Lingual occlusion”.
Abnormal bite as deep bite, cross bite, and edge to edge bite
can be easily recognized. Any premature contact, which may
be caused by tilted or over erupted teeth will prevent the
maximum intercuspation with undue stress and this should
be detected & corrected. Proper mounting is essential to
study occlusion.
III) Occlusal discrepancies & occlusal plane:Some cases
may need to establish a new occlusal plane. With the aid of
radiograph, over erupted teeth can be easily evaluated and
the amount of reduction needed could be determined.
IV) Axial inclination & common path of insertion:Due
to the changes of the tooth axial inclination, some problems may arise in attaining a common path of insertion. With
the aid of radiograph & dental surveyor, the amount of
reduction needed, without endangering the pulp vitality,
can be measured; accordingly the type of the bridge and its
retainers could be selected.
V) Concerning the abutment teeth:
1) Size and form of the coronal portion:-these are well
visualized on the cast, so, we can determine the type of
retainers & the required retentive means.
2) Amount and location of tooth reduction:-on the cast
we can determine the amount of reduction that may be
increased in certain areas.
3) Evaluation of the available tooth structure:-we can
visualize the remaining tooth structure & the occlusal load
imposed on the tooth, after removal of decay.
VI) Alteration of midline:This is easily measured on the
cast & the suitable solution can be reached.
VII) Planning the suitable design:On a second study cast
the suitable design can be visualized & the treatment plan for
the entire mouth is decided.
VIII) Trial preparation and waxing - up:Dentist could
rehearse a proposed treatment plan on another cast. This
enables him to visualize & realize the difficulties that might
face him during tooth preparation. Also through waxing - up,
the final shape of the prosthesis could be properly assessed.
Treatment Planning
Treatment planning consists of formulating a logical
sequence of treatment in steps designed to restore the patient’s
dentition to good health, with optimal function and appearance.
It should be presented in written form & discussed in detail with
the patient.
Successful treatment planning is based on proper
identification of the patient’s need.
A. Treatment is required to accomplish one or more of the following objectives:
- O Correction of existing disease.
- O Prevention of future disease.
- O Restoration of function.
- O Improvement of appearance.
B. Sequence of treatment:
A logical sequence of steps must be decided on - including :- O Treatment of symptoms.
- O Stabilization of deteriorating conditions.
- O Definitive therapy.
- O Program of follow - up care.
I. Treatment of symptoms:The relief of discomfort
attending an acute condition is a priority item in planning
treatment. A fully examination is neither desirable nor
generally possible until the symptoms of the acute condition
have been addressed. Also, urgent treatment of non acute
problems such as a lost anterior crown, a broken porcelain
veneer or fractured R.P.D., should receive priority attention.
II. Stabilization of deteriorating conditions:Such as
dental caries or periodontal disease.
- Replacement of defective restorations.
- Removal of carious lesions.
- Re contouring of over contoured prosthesis.
- Removal of plaque & proper oral hygiene instructions.
III. Definitive therapy:When the stabilization phase has
been completed, successful elective long - term treatment aimed
at promoting dental health, restoring function, and improving
appearance can begin. Several therapeutic proposals may be
applicable to a single patient. The advantages & disadvantages
of each should be thoroughly explained to the patient, with a
diagnostic casts and waxing - up used as guides. Usually oral
surgical procedures are scheduled first, followed by periodontics,
endodontics, orthodontics, fixed Prosthodontics, and finally
removable Prosthodontics.
Oral surgery:The treatment plan should allow time for
healing & ridge remodeling. All preprosthetic surgical procedures
(e.g. ridge contouring) should be undertaken during the early
phase of treatment.
Endodontics:Some endodontic treatment may have been
accomplished as part of the relief of discomfort & stabilization
of conditions. Elective endodontics may be needed to provide
adequate space for a cast restoration or to provide retention for
a badly damaged or worn tooth.
- Orthodontics:Minor orthodontic tooth movement is a
common adjunct to fixed Prosthodontics, especially if tooth loss
has been neglected & drifting has occurred.
- Fixed Prosthodontics:Is initiated only after the preceding
modalities have been completed. This will permit modification
of the original plan , as unforeseen difficulties should surface
during treatment.
+ Occlusal adjustments:are often necessary before the
initiation of fixed Prosthodontics. Where extensive F.P.D. is to be
provided, an accurate & well-tolerated occlusal relationship may
be obtainable only if a discrepancy between IP & CR is eliminated
first.
+ Anterior restorations:are usually done first because
they influence the border movements of the mandible & thus the shape of the occlusal surfaces of the posterior teeth.
+ Posterior restorations:it is often advantageous to restore
opposing posterior segments at the same time. This permits
the development of an efficient occlusal scheme through the
application of an additive wax technique.
+ Complex prosthetics:carefully planned treatment
sequencing is particularly important when complex
Prosthodontic treatments involving alteration of the vertical
dimension or a combination of fixed & removable prosthesis are
required. Two sets of diagnostic casts are accurately mounted, so,
they can be precisely interchanged on the articulator. Definitive
tooth preparation starts in one arch only, preserving the occlusal
surfaces of the opposing arch to act as an essential reference
for mounting the working cast. The definitive restorations are
waxed against the diagnostically waxed cast, establishing optimal
occlusion. When one arch has been completed, the opposing cast
can be restored, achieving the predicted result.
- Removable Prosthodontics:Are the final procedures, but
start to be planned for during fixed Prosthodontic treatment.
- Follow up:A specific program of follow up care and regular
recall is an essential part of the treatment plan. The aim is to
monitor dental health, identify the signs of disease early, and
initiate prompt corrective measures as necessary.
IV.Clinical Tips:
Factors affecting the selection of prosthesis type:
(I) Biomechanical Considerations
1) The decision to remove a tooth:Is part of the
treatment planning process & is made after the advantages
& disadvantages associated with retention of the tooth have
been assessed.
2) The edentulous span:
a- Distribution:
+ Cases with free end saddle will usually require a R.P.Ds..
Alternative treatment are:
- - A distal fixture with implant.
- - Cantilever bridge in selected cases.
- + Multiple edentulous spaces, though each of which may be restored with a fixed bridge, yet due to expenses & technical complexity, a R.P.Ds. May be used.
b- Length:All fixed bridges, long or short, possess a certain
degree of bending when subjected to load; the longer the
span, the greater the flexing.
Bending varies directly with the cube of the length &
inversely with the cube of occluso-gingival thickness of the
pontic considering other factors being equal.
+ Excessive flexing or bending under occlusal force may lead to:
- - Fracture of porcelain veneer
- - Connector breakage
- - Retainer loosening
- - An unfavorable soft tissue response
+ To minimize bending:
- - Construct pontics & connectors of greater occluso-gingival dimensions
- - Use an alloy of higher yield strength
- + Clinical considerations of the bridge flexing in treatment planning:
- - The length of the edentulous area will affect the type of restoration to be suitable for replacing one or two missing teeth.
- - Three posterior teeth is better to be replaced with R.P.D. as F.P.D. will be very questionable.
- - Constructing a long span F.P.D. on short teeth is expected to have a very disappointing prognosis. + Alternative treatment modalities for long edentulous span:
- An implant supported F.P.D. {requires sufficient alveolar bone, broad flat ridge & favorable opposing occlusion}.
- - Removable partial denture.
c- Arch form: The arch curvature affects the amount of
stresses occurring in F.P.Ds constructed in the anterior segment,
especially in the upper teeth.
In cases of pointed arch (V-shaped), pontics of F.P.D would
lie far outside the inter abutment axis line, thus acting as lever
arm producing torque movement on the supporting abutment. +
Measures to be taken in bridge design: If the distance between
the inter abutment axis & the pontic is increased = the force arm
will be increased; this will need to increase the number of the
abutments, to increase the resistance arm for this force.
(II) The Prospective Abutment:
1) The pulpal condition:
a- Vital sound tooth:the unrestored vital caries-free tooth
is an ideal abutment as it facilitates conservative preparation
for strong retentive restoration with good esthetics.
b- Carious tooth:after caries removal as well as all the
undermined enamel, assessment of the remaining sound
tooth structure & the pulpal condition should be performed.
The existing situation would influence the line of treatment
as following:
- + Selecting the most suitable type of restorative material & the necessary retentive means {e.g. pins, grooves or boxes}.
- + Doubtful pulpal condition or those teeth with pulpal capping should not be used as F.P.D abutments unless being endodontically treated.
c- Endodontically treated abutments:A perfectly
endodontically treated tooth (clinically & radio- graphically)
can be used successfully as an abutment with a post & core
for retention & strength.
- + Clinical consideration of endodontically treated abutments:
- - As posts & cores are usually constructed to compensate for the lost coronal part, thus extreme care is needed to get sufficient retention from the post.
- - Before deciding an endodontic treatment for a tooth to be used as abutment, it should be evaluated whether this tooth is restorable or not.
- - In complex & expensive prosthesis whose success is dependent on an abutment that will require endodontic treatment, endodontic surgery or implants may be a better treatment choice.
2) Coronal variations and tooth alignment:
a- Over erupted teeth:to restore the dentition to complete
function, free of interference, over- erupted teeth should be
adjusted to the normal occlusal plane. In some situations
intentional RCT may be necessary to permit enough
shortening to correct the occlusal plane.
b- Short crowns:abutments with short clinical crown would
create problems in constructing F.P.Ds. Careful selection of
the bridge design, with suitable retentive retainers & types
of pontics should be highly stressed on. Considerations in
bridge design:
- - F.-F. Bridge is the most indicated type.
- - Full coverage retainer with additional retentive means are to be used.
- - Establishing relative least convergence.
- - Extend stump of preparation more cervically.
- - To avoid excessive shortening = occlusal reduction to receive retainer with occlusal metal coverage. - Pontics & connectors should be of considerable occluso-gingival dimension to resist bending.
- - Replacing missing 2 or 3 teeth in short occluso-gingival edentulous areas with R.P.D should be highly considered.
c- Mesially tilted 2nd molar:early loss of 1st mand. molar
would create problems if the space is ignored, as mesial tilting
of the 2nd molar. Constructing of F.P.D would face the problem
of attaining a common path of insertion. Different treatment
modalities:
- Up-righting the tilted abutment orthodontically then normal F.-F bridge is considered the treatment of choice.
- A proximal (mesial) ½ crown can be used as a retainer on the tilted abutment.
- F.-S bridge with non rigid connector on the distal aspect of the premolar; so, the path of insertion of the bridge is parallel to the tilted molar. ]
- F.F bridge with telescopic crown on the distal abutment.
+ Telescopic crown is consisted of:
- Thin thimble crown that prepared, constructed & cemented
alone parallel to the long axis of the tilted abutment.
- The external surface is especially designed to be covered by
the retainer of the bridge, which will not cover the distal surface
as it will be inserted parallel to the normal path of insertion.
Mouth preparation
It has become clear that failures are often attributed to
inadequate mouth preparation. In this case mouth preparation
refers to the dental procedures that need to be accomplished
before fixed prosthodontics can properly be undertaken. This is
because the etiologic factors that lead to the need for F.P.Ds, also
promote other pathologic conditions. F.P.Ds will be successful
only if restorations are placed on well restored teeth in a healthy
environment.
Comprehensive treatment planning will ensure that mouth
preparation is undertaken in a logical & efficient sequence,
and aimed at bringing the teeth & their supporting structures
to optimum health. Equally important is the need to educate
& motivate the patient to maintain long-term dental health
through meticulous oral hygiene practices. As a general plan, the
following sequence of treatment procedures in advance of F.P.D
should be adhered to:-
- Relief of symptoms {C.C.}
- Removal of etiologic factors {caries & deposits}
- Repair of damage
- Maintenance of dental health
+ A typical sequence in the treatment of a patient presenting
with extensive dental disease, could be as follows:
- - Preliminary assessment
- - Emergency treatment for symptoms {C.C.}
- - Definitive data collection & assessment of needs
- - Oral surgery
- - Caries control & replacement of defective restorations
- - Endodontic treatment
- - Definitive periodontal treatment, possibly in conjunction with preliminary occlusal therapy
- - Orthodontic treatment
- - Definitive occlusal treatment
- - F.P.D. treatment
- - R.P.D. as immediate transient before implant treatment or permanent restoration
- - Implant treatment
- - Follow up care
Oral Surgery
Oral SurgeryAny abnormality that may
require surgical intervention.
- + Elective soft tissue surgery may include:
- - Alteration of muscle attachments
- - Removal of soft tissue wedge distal to molars
- - Increase of the vestibular depth
- - Modification of edentulous ridges to accommodate F.P.Ds. or R.P.Ds.
B- Hard tissue procedures:It should be performed as
early during treatment as possible to allow the maximum time of
healing & osseous recon touring.
- + It may include:
- - Simple tooth extraction or remaining roots removal
- - Tuberosity reduction or, max. or mand., tori excision
- - Impacted or unerupted supernumerary tooth or 3rd molar removal
C- Orthognathic surgery:Patients who are candidates for
orthognathic surgery require3 careful restorative evaluation &
attention before treatment. Otherwise, an expected improvement
in the facial skeleton may be accompanied by unexpected
occlusal dysfunction. After surgery, the connection between
plaque control, caries prevention, and periodontal health should
be stressed to the patient.
D- Implant-supported fixed prosthesis:Successful implant
dentistry necessitates that both, the patient be meticulously
selected & the technique chosen be skillfully executed.
E- Caries and Existing Restorations
Generally, when a crown is needed, the dentist should
plan
to replace any existing restorations. Although, most teeth will
require foundation restorations, & small defects resulting from
less extensive lesions, can often be incorporated in the design of
a cast restoration or be blocked out with cement. Assessment is more
difficult when an existing crown or F.P.D is being replaced.
Then the extent of damage can be seen only after the defective
restoration has been removed.
+ Foundation restoration or core: Is used to build a damaged
tooth to ideal anatomic form in advance of it’s being prepared for
a crown. It should provide the patient with adequate function &
be contoured and finished to facilitate oral hygiene. Subsequent
tooth preparation is greatly simplified if the tooth is built up to
ideal contour.
+ Selection criteria of the foundation material depends on:
- The extent of tooth destruction.
- The overall treatment plan.
- Operator preference.
It is important to consider the effect of subsequent tooth
preparation for the cast restoration on the retention & resistance
of the foundation. Retention features such as grooves or pins
should be placed sufficiently pulpal to allow adequate room for
the definitive restoration. Adhesive retention may be helpful in
preventing lose of the foundation during tooth preparation.
F- Endodontics:
- + Assessment: the clinical examination should include:
- - Tenderness to percussion should be noted.pulpal health.
- - Any abnormal sensitivity, soft tissue swellings, fistulous tracts, or discolored teeth.
- - Carefully examined radiographs for signs of periapical disease, if there is doubt concerning pulpal health.
+ Treatment:it should be a general rule to perform
conventional rather than surgical endodontics, if possible;
because apicoectomy adversely affects the crown/root ratio &
thus the support of the planned prosthesis. When a post & core
restoration is needed, 3-5 mm of apical seal should be retained.
The post can usually be removed to access recurrent periapical
lesion, using a “ Masserann Kit “. It may be desirable to perform
elective endodontics in the following situations:-
- When there are problems in obtaining a completely compatible line of withdrawal between multiple abutments.
- When it is impossible to gain adequate retention in a badly worn tooth.
- When the pulpal prognosis of an abutment tooth is compromised & additional preparation is likely to further jeopardize its longevity.
G- Definitive Periodontal Treatment:Certain specific
periodontal procedures may be indicated to improve the prognosis of a restoration.
H- + Mucosal reparative therapy:It is recommended that
a tooth to be treated with restoration extending into the gingival
sulcus should have approximately 5 mm of keratinized gingiva, at
least 3 mm of which is attached gingiva. Where less keratinized
gingiva is present, or in areas of localized gingival recession, a
grafting procedure should be considered.
- - Free autogenous gingival graft.
- - Laterally positioned pedicle graft.
- - Coronally positioned pedicle graft.
- + Crown lengthening procedure:- May be indicated:
- To improve the appearance of an anterior tooth.
- When the clinical crown is too short to provide adequate retention without the restoration’s impingement on the soft tissue { biologic width }.
- In some patients with extensive sub gingival caries, sub gingival fracture, or root perforation resulting from endodontics.
When crown lengthening is the treatment of choice it may be
accomplished either surgically or with combined orthodonticperiodontic
techniques depending on the patient & dental
situation.
I-Orthodontic Treatment:
Minor orthodontic tooth movement can significantly
enhance the prognosis of subsequent restorative treatment.
Up righting of malpositioned abutment tooth can improve axial
alignment, create more favorable pontic space, and improve
embrasure form in the fixed prosthesis. Additionally, it can direct
occlusal forces along the long axis of the tooth & often lead to a
substantial conservation of tooth structure.
J- Definitive Occlusal Treatment:
Mouth preparation often involves reorganization of the
patient’s occlusion, typically to make IP coincide with CR &
remove eccentric interferences. The coincidence of CR & IP
greatly facilitates accurately transferring the patient’s casts to an
articulator. When selective grinding of the natural dentition is
being considered, it should be remembered that this is a purely
subtractive procedure (tissue is removed) and is limited by the
thickness of the enamel.
Obviously, before any irreversible changes are made in the
dentition, a careful diagnosis must establish whether indeed
restorations will be needed.
+ Diagnostic adjustment:-2sets of articulated diagnostic
casts are required. One set will serve as a reference; the other will
be used to evaluate how much tooth structure has been removed
and how much more must be removed to meet the objectives of
the procedure. This will reveal the efficacy of the treatment plan before anything is done.
The primary objectives of selective occlusal grinding are:
- To redistribute forces parallel to the long axes of the teeth by eliminating contacts an inclined planes & creating cuspfossa occlusion.
- To eliminate deflective occlusal contact; CR coincides with IP.
- To improve worn occlusal anatomy, enhance cuspal shape, narrow occlusal tables, & reemphasize proper developmental & supplemental grooves in otherwise flat surfaces.
- To correct marginal ridge discrepancies & extrusions, so oral hygiene will be easier.
- To correct tooth malalignment through selective reshaping.
It will not always be possible to achieve every one of these
goals.
If a choice must be made, corrective therapy should not be
at the expense of functional surfaces & should not destroy any
functional contact.
+ Clinical occlusal adjustment:
A- Patient selection:careful analysis of the diagnostic
occlusal adjustment must be made to determine whether the
patient is a good candidate for such irreversible subtractive
treatment.
Precise reduction & close attention to the sequence are
essential. A written record of each reduction is also recommended.
The following should be considered as contraindications to
definitive occlusal adjustment:
- A bruxer, whose habit cannot be controlled,
- When the diagnostic correction indicates that too much tooth structure will be removed.
- A complex spatial relationship [e.g. Angle class II & skeletal class III].
- When max. Palatal cusps contact mand. buccal cusps.
- An open anterior occlusal relationship.
- Excessive wear.
- Before orthodontic or orthognathic treatment.
- Before physical or occlusal appliance therapy.
- A patient with T.M.J pain.
- A patient whose jaw movements cannot be manipulated easily.
B- Occlusal adjustment:it needs to be undertaken in a
logical sequence of steps, so, this will avoid repetition & improve the efficacy of treatment.
The steps are:
(1) Elimination of CR interferences:
mandibular tooth follows its own arc of closure. If IP & CR
positions don’t coincide, premature contacts will be unavoidable.
Manipulate the mand. & mark the tooth, so that, the initial contact
in CR & the extent and direction of jaw movement to IP are
seen. This movement, or slide, can be in either an anterior or a
lateral direction. Find any interference that because the condylar
processes to be displaced & adjust it by selective grinding of the
cuspal inclined planes.
(2) Elimination of lateral & protrusive interferences:
The goal of this phase of adjustment are to eliminate contacts
between all posterior teeth during protrusive movements, mediotrusive [non working], & latero-trusive [working]. In
certain patients, group function of the working side contacts
should be considered rather than the more ideal mutually
protected occlusion; especially when there is mobility, poor bone
support, wear, or malpositioning of the canines. It is essential
during this phase of adjustment, that no centric contacts be
removed. In general, lateral & protrusive interferences are
eliminated by creating a groove that permits escape of the centric
cusp during eccentric movements [1-3].
For more Open Access Journals in Juniper Publishers please click on: https://juniperpublishers.com
For more articles in Open Access Journal of Dentistry & Oral Health please click on:


Comments
Post a Comment