Comparison of Push out Bond Strength of Customizable Fiber Post using two Self Adhesive Resin Cement-An In-Vitro Study- Juniper Publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF DENTISTRY & ORAL HEALTH
Comparison of Push out Bond Strength of Customizable Fiber Post using two Self Adhesive Resin Cement-An In-Vitro Study
Authored by Priti Desai
Abstract
Materials and Methods: Twenty
human mandibular single-rooted second premolar teeth were decoronated,
endodontically treated, post space prepared and divided into two groups
(n = 10); Group I: Everstick post (GC India) and U-200 resin cement(3M),
Group II: Everstick post (GC) and G-cem Resin cement (GC). Each root
was sectioned to get slices of 3 ± 0.1-mm thickness. Push-out tests were
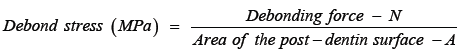
performed using a universal testing machine. To express bond strength
in megapascals (Mpa), load value recorded in Newton (N) was divided by
the area of the bonded interface.
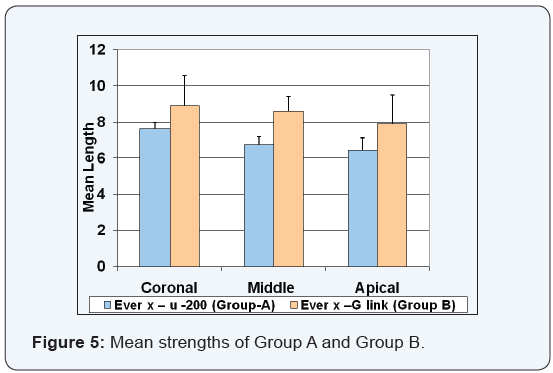
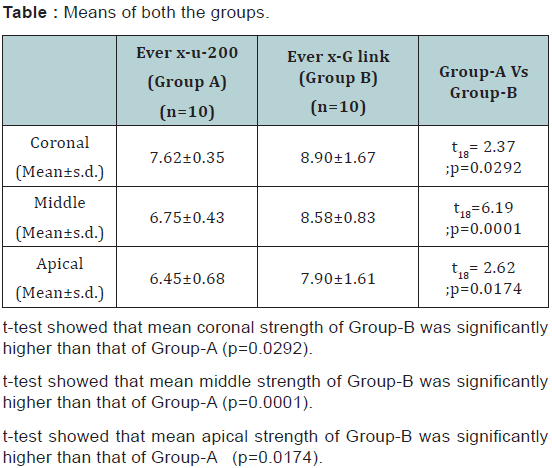
Results: The mean values of the
push-out bond strength show that Group II had significantly higher
values than Group I in all three region of the root.
Conclusion: Within limitation
of present study it can be concluded that customizable post shows good
bond strength with respective resin cement from the same manufacturer.
Abbreviations: GC: G-cem
Resin Cement; Mpa: Mega Pascals; N: Newton; FRC: Fiber-Reinforced
Composite; SARCs: Self-Adhesive Resin Cements; IPN:
Semi-Interpenetrating Polymer Network; PMMA: Polymethyl MethacrelateIntroduction
Endodontically treated teeth, with a large amount of
coronal tooth structure missing, frequently require the placement of a
post inside the root canal, to retain a core for definitive restoration.
The choice of appropriate restoration for these teeth is influenced by
strength and esthetics. Depending on the clinical parameters, the choice
may be a metal or an esthetic post and core restoration.
Fiber-reinforced composite (FRC) posts, as an alternative to cast post
and cores and metal dowels, were introduced in the early 1990s to
restore endodontically treated teeth with an excessive loss of tooth
structure [1,2]. The popularity and preference for FRC posts can be
chiefly ascribed because of an elastic modulus that is closer to that of
dentin and provision of good esthetic particularly when all ceramic
crowns are done [3]. Other advantages of FRC posts include enabling
smooth cementation procedures to be carried out without friction with
root canal walls and a reduced risk of root fractures [1-5]. Later on
several advantages are shown in an in-vitro studies that FRC posts
distribute occlusal stresses more evenly in the root dentin, thereby
resulting in fewer and more favorable root fractures, which were often
repairable [6-8].
When post and core restoration done in esthetic
region of mouth, quartz or glass fiber posts can be used [9]. With
regard to the fiber posts that are currently available on the market,
they are composed of unidirectional fibers embedded in a resin matrix in
which reinforcing quartz or glass fibers are immersed. Fibers are
pre-stressed, and subsequently resin (as a filler) is injected under
pressure to fill the spaces between the fibers, giving them solid
cohesion [10,11]. Because of rigidity and poor adaptability of FRC post
and more chances of debonding of fiber reinforced post recently
customizable fiber post are introduce in market that are flexible during
manipulation and rigid after light curing that makes them adopt well to
root canal anatomy .e.g. Everex post, Peerless Post etc.
With the newly developed self-adhesive resin cements,
no pre-treatment of dentin conditioning with the phosphoric acid is not
required, so the step of rinsing off the phosphoric acid is also
eliminated, and hence the need for clinical assessment of optimal dentin
wetness after rinsing dentin [12]. In other words, the simpler
self-etching adhesive approach requires a reduced number of clinical
procedural steps, hence offering the advantages of a shorter adhesive
application time and more importantly, reduced technique sensitivity. As
for the bonding
performance of self-adhesive resin cements when used to lute
fiber posts, it has been assessed in in-vitro studies and compared
against the performance of total-etching adhesive. However,
findings on the performance of self-etching adhesives with
regard to customized fiber post cementation were not consistent
in literature search.
So here with we have done study to find push out bond
strength of customized post with different self adhesive resin
cement. The aim of the present study was to do comparative
evaluation of the push-out bond strength of two new selfadhesive
resin cements (SARCs) used for luting customizable
glass fiber posts into root canals obturated with resin-based
sealer (AH 26) and core material (Gutta-percha).
The null hypotheses tested were as follows:
Materials and Methods
Twenty human mandibular second pre-molars extracted
for periodontal and orthodontic reasons were selected. The
specimens were free of cracks, carious lesions, fractures, and
resorption, with fully developed apices and without previous
endodontic treatment. Teeth were cleansed using ultrasonic and
disinfected by immersion in 2.5% sodium hypochlorite solution
for 2hr and stored in normal saline (Figure 1). All the teeth were
decoronated 1.5-2.0mm coronal to the cemento–enamel junction
with a diamond disc to get 15 mm root length. The pulp tissue
was extirpated and canal patency was assessed with a size 10
K-file. Working length was established 1 mm short of the apical
foramen and canals were enlarged up to rotary protaper F3
file following the crown down technique with an intermittent
irrigation using 1ml of 2.5% sodium hypochlorite. After final
irrigation with normal saline, the canals were completely dried
and obturated using AH plus sealer and corresponding F3 Guttapercha.
Followed by temporary seal and stored for saline.

Post luting procedures according to adhesive approaches
For post space preparation, temporary seal and gutta-percha
was removed with a warm plugger and peeso file no 3 (1.1mm
diameter), leaving a minimum apical seal of 4−5 mm of guttapercha
in the canal. Post holes were prepared up to a depth
of 10mm from the CEJ. A final flushing of the canal space was
accomplished using sterile water, and the canals were dried with
paper points (Dentsply-Maillefer). The presence of any residual
gutta-percha in the root canal walls along the post space was
checked by radiographic evaluation. Customizable post were
customized for each tooth before curing it according to shape
of canal in each specimen (Figure 2). The prepared specimen
roots were randomly divided into two groups: Group-1, Group-2.
In group-1 the resin cement used was U-200 resin cement
and in group-2 G-cem link ace resin cement were used. Before
cementation all the specimen was cleaned, rinsed and the post
space was thoroughly dried using paper points. Cementation
is done with direct method means preshaped customized post
(Everstick post, GC India) placed in canal after placing respective
cement in specimen root and post and curing for both done
together) using Automix Tip for Endo with extension tip which
extrude material into root canal and post was insert immediately
within 1min. excess cement was removed and light cure for
20sec was done. After curing specimen roots were stored in
normal saline for 72 hours.
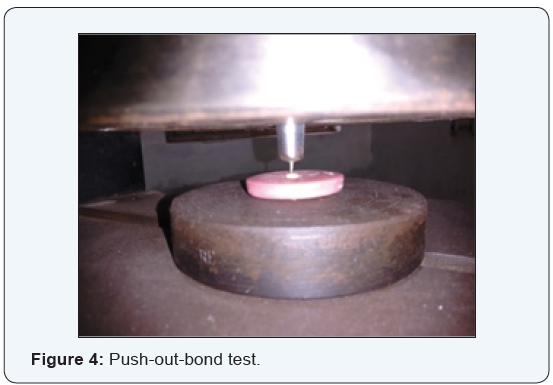
Push-out bond strength evaluation
To evaluate the push-out bond strength between the fiber
posts and the luting cements, a thin-slice push-out test was used
in this study. Each specimen was sectioned horizontally with a
low-speed diamond disk (Isomet 1000, Buehler Ltd.) under water
cooling to produce three 3±0.1 mm thick post-dentin sections
from CEJ to apical third (cervical, middle, and apical) (Figure
3). The first slice represented the cervical region, the next slice
represented middle region and the last slice represented the
apical region of the prepared post space. None of the slices failed
during sectioning, and all slices were used for push-out bond strength evaluation. Each specimen was marked on its coronal
surface with an indelible marker, and the exact thickness of each
slice was measured using a digital caliper (0.01 mm accuracy;
Mitutoyo, Tokyo, Japan).

Each section was attached to a push-out jig with a cyanoacrylate adhesive (Zapit®, Dental Ventures of America Inc., Corona, CA, USA), whereby the coronal surface of root faced the jig and the post was centered over the hole of the jig. The post segment was loaded with a custom made jig (1mm in diameter), which was centered on the post segment and which had no contact with the surrounding dentin surface. Load was applied with a universal testing machine, in an apical-tocervical direction with respect to the individual test specimens, at a crosshead speed of 1mm/min until the post was dislodged (Figure 4). Push-out bond strength was measured in Kilo Newton converted to megapascals (MPa) for each specimen by using the following formula: (Table 1 & 2) (Figure 5).

Discussion
The success of endodontic therapy depends on adequate post
endodontic restoration to make pulpless teeth function as an
integral part of the masticatory apparatus. Pulpless teeth present
various challenges of the restorative problems such as loss of
tooth structure by caries or fracture and previously existing
defective restorations. The introduction of the intracoronal
post in endodontically treated teeth serves primarily to retain
core structure and later coronal restoration. Many different
types of posts have been used such as, cast metal alloy posts
and prefabricated metal posts made of various alloys such as
stainless steel and titanium. The cast post core system needs
elaborate laboratory procedures and have rigidity due to its high
modulus of elasticity and that is the major drawback of metal
posts. Catastrophic root fractures have been attributed to these
differences in the rigidity of the post and root dentine due to
stress concentrations inside root leading to irreparable failures.
In recent years, non-metallic posts with biological and physical
properties similar to that of dentine have been introduced.
The advantages claimed for fiber posts are that post can
be bonded to the tooth, and modulus of elasticity is close to
that of dentin resulting in greater post flexibility. To preserve
esthetics, fiber posts have been introduced, which are made
of quartz and glass fibers embedded in a resin matrix. These
posts are composed of unidirectional fiber and are becoming
more popular because of their good bond strength to dentine
and light transmission. An in-vitro study suggested that fiber
posts are less likely to cause vertical root fracture as compared
to stainless steel posts because forces are apparently absorbed
by the post and core and not transferred to the root structure.
The most common disadvantage of post cores is poor retention
of posts, debonding is common problem. The post material,
surface structure, post length cement, luting cement and amount
of remaining tooth structure all affect retention of the post. In order to improve bond strength between the post and resin
cement, many post surface pre-treatment procedures have been
suggested regarding the use of mechanical or chemical agents
[10].In-vitro studies regarding effect of cement on retention of
post has been investigated extensively. Studies have shown that
use of resin cement significantly increases retention and fracture
resistance of tooth by providing adhesive bonding.
The retention of fiber posts in root canals is dependent upon
adhesion between the resin cement and the dentine, as well as on
adhesion between the resin cement and the posts. However, the
adhesion between the resin cement and the dentine is considered
to be the weak point in luting a fiber post [13]. Although bonding
between the post and the root canal dentine plays a pivotal role in
the long-term success of a restoration, ensuring reliable bonding
between the post and the composite core is also necessary. If the
bonding of that interface is poor, de-bonding and/or fracture of
the core and post can occur [14]. Successful bonding minimizes
the wedging effect of the post within the root canal and requires
less dentine removal to accommodate a shorter and thinner
post; in addition, it leads to lower susceptibility to tooth fracture
[15]. Bonding to root canals might be difficult, because of the
handling characteristics of the adhesive system, root anatomy,
tooth position, the use of a light-curing technique, the experience
and skill of the operators, etc [16].
Self-adhesive cements were introduced in 2002 as a new
subgroup of resin cements [16]. They were designed with the
intent of integrating the favorable characteristics of different
cement classes into a single product [17]. Their main advantage
is the simplicity of clinical use. These cements are expected to
offer properties analogous to those of resin cements.
The results of this study require the rejection of the
null hypothesis since differences in push-out bond strength
exist between the tested self-adhesive cements. The bonding
mechanism of self-adhesive cements rely on chemical interactions
and micromechanical retentions with the bonding substrate, but
concerns still exist on the effective adhesive potential of these
simplified cements. In the present study, G-cem link ace attained
higher bond strength values when compared to Rely X U-200. A
variety of experimental tests has been described for evaluating
the strength of the bond between the root canal dentine and
the fiber posts, such as the pull-out test, the microtensile test,
and the push-out test [18-20]. In the present study, the pushout
test was performed using 1mm thick tooth slices, because
this approach offers the advantage of smaller adhesive areas,
which help to avoid the difficulties of microtensile specimen
preparation. Cylindrical or conical fiber posts may be used in the
push-out test procedure. In both cases, the result is a complex
stress distributed at the interface between the dentine and the
resin cement and between the post and the cement with a shear
stress component [20]. Cylindrical posts used in the push-out
test have been reported in some studies to increase the risk of
friction [21]. Conical fiber posts with a shape more appropriate for root canal preparation will eliminate some of the friction
between the resin cement and the post from the push-out test.
This is why customizable fibre post (Everex Fiber Post) was used
in the present study for evaluation of the push-out bond strength.
In both groups coronal bond strength was higher than middle
third and middle third has higher bond strength value than apical
third. Our result was in agreement with the previous studies that
reported higher bond strength for coronal dentin than values
for the middle and apical sections of the root. Prefabricated post
are made up of highly cross link polymer matrix between fiber
because of high conversation rate they should be more or less
non reactiven therefore bonding between prefabricted post and
adhesive luting agent can be hamphered. Recently developed
FRC post consisit of continous unidirectional glass fibres and
multiphase polymer matrix. This polymer matrix reveals a
semi-interpenetrating polymer network(IPN) with both linear
polymer phases, polymethyl methacrelate(PMMA) and cross
link polymer phase. Monomer of adhesive resin penetrate
in to the linear phases and form an interdifusion bonding by
polymerization [22].
Kerstin Bitter et al. [23,24] in 2007 done study investigated
bond strength of ever stick post with different resine cement
using push out model. Type of post and cemtent used has
signifcant effect on bond stregth of fiber reinforced post.
IPN everstick post shows good bond stregnth compared to
prefabrcated post. The surface of prefabricated fiber post with
cross link matrix has very small amount of reactivity is left for
free radical polymerization and bonding,lead to lower bond
stregnth with prefabicated FRC post than customizsed FRC post.
In customised post linear (PMMA) and cross link phases both
are present, linear phase is penetrated ny Bis pheno-A glycidyl
methacrylate of resin cement and inter difussion bonding is
established, lead to high bond stregnth of everstick post. Failure
mode between prefabricated FRC post and customised post
is found poor adhesion between resin cement and post.post
composite bond is poor rather than resin cement or post itself.
Type of Resin ceement used significantly affect the bond strenght
of FRC post but type of post use has more influence on the bond
stregnth of post [23].
There are two types of technique are used for cementation
of FRC post, indirect (post is cure before cementation and direct
technique (post and resin cemented cure together). The “direct
technique” seems to be beneficial when cementing individually
formed FRC posts than indirect technique (polymerized before
cementation). Bonding of a FRC root canal post to a root depends
on the adhesion of luting cement to the post and to the root canal
dentin [24]. According to Davis et al. [25] the flexural strength
of the Stick Tech post was significantly lower than the flexural
strength of the GC post. The mode of failure for the GC Posts
was adhesive, whereas the Stick Tech posts failed cohesively.
Different flexural strengths and failure modes were observed
among the two fiber post-resin systems [25].
Conclusion
Within limitation of the study it can be concluded that
the post system and resin cement should be used from same
manufacture company.
For more Open Access Journals in Juniper Publishers please
click on: https://juniperpublishers.com
For more articles in Open Access Journal of Dentistry & Oral
Health please click on:

Comments
Post a Comment