Bacterial Adhesion on Zirconia, Lithium Desilicated and Gold Crowns-In Vivo Study- Juniper Publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF DENTISTRY & ORAL HEALTH
Bacterial Adhesion on Zirconia, Lithium Desilicated and Gold Crowns-In Vivo Study
Authored by Abbas I Hussein
Abstract
Zirconia crowns have recently
been used as an alternative to the common gold crowns and as a
competitive to lithium disilicate crowns as well. Many research works
demonstrated that zirconia crowns do not adhere bacteria. In an
experiment carried out on 17 participants from Ramadi rural areas, Anbar
province, Iraq. Participants underwent professional cleaning and
instructed not to brush for 72hours where swabbed were taken by
microbiologist from gold, lithium disilicate and zirconia crown surfaces
and cultured in two Petri dishes of blood and sabouraud agars and
incubated for 48 hours at 37°C. Kruskal-Wallis test showed that median
number of Streptococcus Sanguineous colonies on zirconia crowns was significantly lower than the other two medians. Candida albicans was only found in one case of gold crowns.
Keywords: Zirconia; Gold; Lithium; Biofilm; Adhesion
Introduction
Gold alloys are traditionally used in dental
application for many decades. The main use of this material is to build
full crowns. The increased price of gold led to decrease demands on this
material [1]. The search for new materials to replace gold leads to the
introduction of material sat reasonable price. Lithium disilicate (IPS
e.max, Ivoclar Vivadent) is a glass-ceramic, which claims to combine
high flexural strength along with optimum esthetics [2]. Zirconia
(zirconium oxide) was introduced by Martin Heinrich Klaproth in 1789
[3]. This material is believed to be a non-cytotoxic metal oxide,
insoluble in water and has no potential of bacterial adhesion. In
addition, this material has radio-opacity properties and exhibits low
corrosion [4,5]. In the last decade of the 20th century,
yttrium oxide partially stabilized tetragonal zirconia polycrystals
(Y-TZP) was introduced to dentistry as a core material for all-ceramic
restorations and has been made available through the CAD/CAM technique
[6]. Since then many attempts had been made to improve mechanical
properties of zirconia as well as to enhance its biocompatibility.
Recently, different types of zirconium have been mentioned in many
scientific articles as suitable choice for dental restorations due to
their good mechanical properties, tooth-colored and natural appearance
and low plaque accumulation [7-9]. According to the potential extension
of using zirconia oxide in dental restoration, it is of interest to
continue searching the ability of this material to resist bacterial
adhesion. In this context, the main aim of this research work was to
investigate whether or not this material is not adhering bacteria
accumulated on crown surface. Adhesion of bacteria to the surfaces of
both removable and fixed partial dentures can be considered as an
important health issue that many authors reported its potential to cause
various diseases and illness. Many researchers have studied this
problem as to show the types and intensity of bacterial accumulation on
the surfaces or bases of dentures [10-12].Al though many articles
emphasized the property of zirconia to not adhere bacteria and or fungi,
but this is not absolute. Although the number of bacterial colonies on
zirconia crown surface were the lowest, but it indicates the possibility
of adhering bacteria. From personal observation and daily communication
with bacteriologists, it is important to keep in mind that bacterial
adhesion does not necessarily relatetothe dental materials only, but it
is also a matter that relate to different socio-economic factors such
as; standard of living, food habits, educational level, residential
area, and the general attitude of people on their general health.
The adhesion of bacteria on any surfaces of teeth
will form a biofilms which can be a good environment for many
microorganisms such as algae, protozoa, and many fungi. The success of
dental restoration therefore will be due to the success of avoiding
biofilm formation. There are two main points in this context; the first
point is the dental material used in restoration, and the second point
is the patient. With regard to the first point, scientific research has
to continue in order to find a certain material
that is absolutely or at least most likely not adhere bacteria. This
is really a very difficult task but it is necessary to save efforts,
time, and money. According to the second point, patients must
be informed that bad foods habits, bad commercial tooth paste,
and improper tooth cleaning may failure of dental restoration.
Patients and Methods
As to investigate how dental materials are differ in their ability
to adhere bacteria and or fungi on their surfaces, three main
dental materials were considered. These are; gold alloy, lithiumdesilicated,
and zirconia-based ceramic. A sample of 17 patients
were randomly selected from patients living in rural areas of Ramadi
city, Anbar province, Iraq. All of them were visiting private
dental clinics during the period April-August 2013. The selection
criteria were that; all patients must not suffer from any chronic
diseases, did not take any type of drugs for the last month,
and fixed partial dentures should not be exceeds one year of use.
Prosthesis was in the maxillary arch. All of them were instructed
in advance how to participate in this research work. Participants
had been told about the main aim of this research work.
Everyone was scheduled on two occasions; the first occasion
when participant undergo a professional tooth cleaning at the
clinic, and the second occasion when professional microbiologist
is ready to take biofilm swabs. After finishing professional
tooth cleaning, participants were instructed to eat as usual and
not to brush their teeth 72 hours before the next visit. At this
time bacterial formation can be observed. During the next visit,
two procedures were adopted. The first procedure was the visual
evaluation food residue on the crown surface which was done
by the dentist on a scale of four degrees, 0 (no food residue),
1(slight residue), 2 (moderate residue), 3 (intense residue). The
second procedure involved swabs taken by the microbiologist.
Two swabs were taken from every participant. One was cultured
in a standard Petri dish with blood agar and the other one cultured
in Petri dish with sabouraud agar, both were incubated for
48 hours at 37°C.The aim of the first agar was to observe growth
of Streptococcus sanguineous as it is believed that it is the leading
cause of dental plaque, whereas the other agar was to observe
growth of Candida albicans fungus. Identification of the isolates
was very important in order to emphasize whether or not streptococcus
sanguine is the dominant streptococci species or not.
Streptococci species were identified with regard to their characteristics
colonial morphology colonies in blood agar Gramstained
smears and catalase test. Colony forming unit (CFU) was
used to estimate the number of differentiated bacterial colonies.
The software SPSS version 17 was used to analyze the collected
data analysis of variance (ANOVA).
Results and discussion
Patients’ age ranged between 38-48 years, with mean age of
43.23 years and standard deviation of 2.73 years. The sample involved involved
10 women (58.82%) and 7 men (41.18%). The one-way
analysis of variance showed that there is no significant difference
between groups’ mean age (Table 1), which is an evidence
to discard age effects on the process of bacterial accumulation.
It is very clear from personal observation that as age increased
people become more careless about their own dental health
status as a common behavior in most Arabic countries. Such a
behavior will leave a print of its bad impact on many real dental
problems like plaque and caries which probably lead to loss
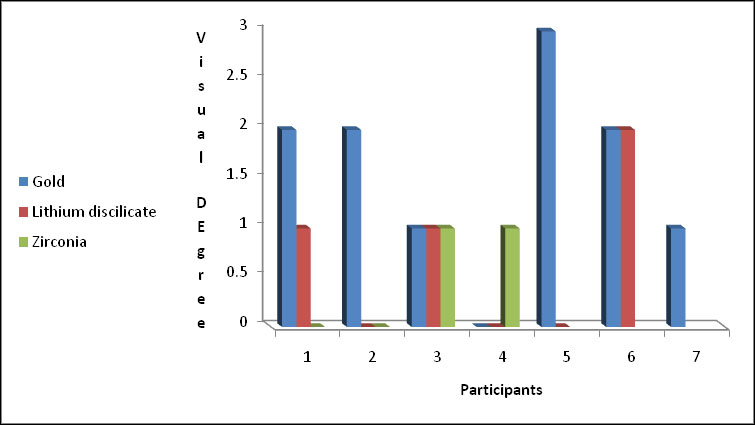
natural teeth. Figure 1 shows the visual evaluation of the food
residue as observed clinically by the dentist. The figure showed
clear accumulation of food residue on gold material in comparison
to the other two materials which reflect the ability of
this material to adhere such particles. The Kruskal-Wallis’ test
showed that there is no significant differences (p>0.05) when
comparing groups median of the evaluation degree for the three
materials. Nevertheless, when considering lithium disilicate and
zirconia as a one group and comparing them to gold by the use
of Mann-Whitney’ test a significant difference (p< 0.05) between
median visual evaluation degree was obtained. Lithium disilicate
and zirconia crowns are less susceptible to adhere bacteria than
gold. This is of course indicated that appearance of zirconia and
lithium silicate surfaces are much better than that of gold. It is a
good advantage that these materials help wearer to have good
teeth looking. Table 2 shows the number of streptococcus sanguineous
species as determined from cultured swabs. The Kruskal-
Wallis test showed that median streptococcus sanguineous
colonies are significantly different (p< 0.05) between groups of
crown materials. Gold crowns found to adhere the highest number
of bacterial colonies followed by lithium dislocate. Zirconia
crowns appear to adhere the minimum number of bacterial colonies.
It may be possible that with daily tooth brushing zirconia
crowns may not be susceptible to adhere any bacteria for
short time. However, bio film may be accumulated on zirconia
surfaces in longer time than it does on other material surfaces.
Candida albicans fungi are found only in one case of gold crown
participants. This is may be because gold crowns surfaces are
not smooth enough like surfaces of the other two materials, and
that explained how the roughness of materials can construct an
environment for bacteria and fungi
Conclusion
From the results we can conclude that zirconia crowns adhere
less Streptococcus Sanguineous colonies compared to lithium
disilicate and gold crowns. The participants from rural areas
are considered at the lower level of people who are caring about
oral hygiene. In this context, any material could be exposed to
the risk of biofilm formation which lead by time to number of
dental diseases in addition to the potential corrosion of the
dental restoration. Zirconia crowns is still not common due to
its expensive price in comparison to other materials. Moreover,
the slight potentiality of bacterial adhesion may not make it as a
competitive material to the other available counter parts materials.Effort and research must be continued to achieve zirconium
alloys which provide both, cheap and higher biocompatibility
that ensure the lowest potentiality of adhering bacteria.
Figure 1: Visual evaluation of food residue.
For more Open
Access Journals in Juniper
Publishers please click on: https://juniperpublishers.com
For more articles in Open Access Journal of Dentistry & Oral
Health please click on: https://juniperpublishers.com/adoh/classification.php

Comments
Post a Comment